
Why would a patient with a wound spend almost 2 hours a day, 5 days a week, in a locked chamber rece…

The goal of wound-bed preparation is to create a stable, well-vascularized environment that aids hea…

Nurses and therapists often wonder if their license permits them to perform sharp wound debridement.…

Using maggots to treat wounds dates back to 1931 in this country. Until the advent of antibiotics in…

Optimizing nutritional status is a key strategy both in preventing and managing pressure ulcers. In …

Support surfaces are consistently recommended for the prevention and treatment of pressure ulcers. S…

Developing a pressure ulcer can cause the patient pain, lead to social isolation, result in reduced …

As a wound care specialist, you have learned about many skin conditions, some so unusual and rare th…
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Having the proper support surface for beds and wh…
By Ann-Marie Taroc, MSN, RN, CPN
Are you using the wrong kind of medical tape on your patients? A…

By Todd Zortman, RN, WCC, and James Malec, PhD
Pressure ulcers are a chronic healthcare burden fo…

By Janet Wolfson, PT, CWS, CLT-LANA
After landing my dream job as the wound care coordinator at a…
By Cindy Barefield, BSN, RN-BC, CWOCN
Like many hospitals, Houston Methodist San Jacinto Hospital…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
Research has shown that exercise can help ease symptoms…
By Karen Culp, RN, WCC
I’m one of the nurses responsible for the pressure ulcer prevention educati…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
A declining pressure ulcer decreases the quality of life…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
The challenge of preventing pressure ulcers is won thro…
By Susan Beard, RN, BS, CWOCN
Suppose you’re reading an article on a new product that states the …
By Catherine E. Chung, PhD, RN, CNE, WCC
As a wound care clinician, you teach patients about medi…
By Stanley A. Rynkiewicz III, MSN, RN, WCC, DWC, CCS
Developing a successful wound care program r…
By David L. Johnson, NHA, RAC-CT
As a senior quality improvement specialist with IPRO, the Qualit…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
As a wound care nurse, do you feel the weight of the wo…
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Welcome to our second annual “Best of the Best” i…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
The development of a care plan related to skin integrit…
By Judy Bearden, MSN/ED, RN
Changes in healthcare policy and reimbursement are pushing treatment …
By Catherine R. Ratliff, PhD, APRN-BC, CWOCN, CFCN
It’s estimated that about 70% of the 1 million…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
Prevention of pressure ulcers and skin breakdown begins…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
We’ve all experienced how a bad night’s sleep can affec…
By Jennifer Oakley, BS, RN, WCC, DWC, OMS
I used to think I could do it alone. I took the wound c…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
As wound care clinicians, we know that an interdiscipli…
By Beth Hoffmire Heideman, MSN, BSN, RN, WCC, DWC, OMS
Fifty shades of wound care at home refers …

By Kulbir Dhillon, MSN, FNP, APNP, WCC
Venous disease, which encompasses all conditions caused by…
Aresolution is a serious decision or determination to do, or not to do, something. Traditionally, mo…
By Lydia A. Meyers RN, MSN, CWCN
Missed care, a relatively new concept in the medical community, …

By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS
Each issue, Apple Bites brings you a tool you c…
By Robyn Bjork, MPT, WCC, CWS, CLT-LANA
Margery Smith, age 82, arrives at your wound clinic for t…
By Ronnel Alumia, BSN, RN, WCC, CWCN, OMS
Achieving excellent wound care outcomes can be challeng…
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
The first 24 hours after a patient’s admission are crit…
By Janice M. Beitz, PhD, RN, CS, CNOR, CWOCN, CRNP
Quality patient education is essential for com…
Here are some resources of value to your practice.
National Guideline Clearinghouse
The National G…
By: Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Why is it that the people who are the most carin…
By T. Michael Britton, RN, NHA, WCC, DWC
As wound care professionals, we’ve all experienced a tim…
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Knowledge is exploding online, making it essentia…
by Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
What an honor it is to be the wound care “superhe…

By Robyn Bjork, MPT, CWS, WCC, CLT-LANA
The ability to understand or “read” lower-extremity redne…

By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
With so much focus on dressing choices, it’s easy t…
By Robyn Bjork, MPT, CWS, WCC, CLT-LANA
One of the worst fears of a wound care clinician is inadver…
By Cindy Broadus, RN, BSHA, LNHA, CHCRM, CLNC, CLNI, WCC, DWC, OMS
At one time or another, all woun…
By Robyn Bjork, MPT, CWS, WCC, CLT-LANA
In a busy wound clinic, quick and accurate differential dia…
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Digital cameras have many helpful features, but the…
By Robyn Bjork, MPT, CWS, WCC, CLT-LANA
A hot flush of embarrassment creates a bead of sweat on my …
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
With this PDF, which you can download, you can have…
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Use this handy reference tool to help you assess lo…
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
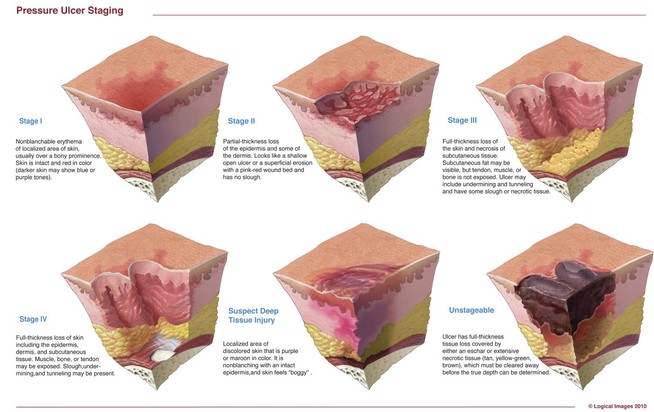
Staging pressure ulcers can be challenging. Below…
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Writing effective orders for wound care is vital to…
By Goranka Paula Bak, BSN, RN, ET, CWOCN
Before discharge, a new ostomy patient and caregiver have …
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Wound pain can have a profound effect on a person’s…
By Susan Reinach-Lannan, BSOM
In the current healthcare environment, wound care practitioners need …
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC
This chart (please click the PDF icon to download) expla…
By Katherine Rossiter, EJD, MSN, APRN-NP, CPNP; and Stephen Lazoritz, MD, CPE
An angry patient is l…
