Optimizing nutritional status is a key strategy both in preventing and managing pressure ulcers. In patients across all care settings, compromised nutrition— as from poor intake, undesired weight loss, and malnutrition—increases the risk of pressure ulcers. It contributes to altered immune function, impaired collagen synthesis, and decreased tensile strength. In many cases, malnutrition also contributes to wound chronicity and increases the risk for delayed and impaired wound healing. In patients with chronic wounds, such as pressure ulcers, a chronic inflammatory state can induce catabolic metabolism, malnutrition, and dehydration. (more…)
Read MoreSearch Results for: Preventing
No more skin tears
Imagine watching your skin tear, bleed, and turn purple. Imagine, too, the pain and disfigurement you’d feel.
What if you had to live through this experience repeatedly? That’s what many elderly people go through, suffering with skin tears through no fault of their own. Some go on to develop complications.
A skin tear is a traumatic wound caused by shear, friction, or blunt-force trauma that results in a partial- or full-thickness injury. Skin tears are painful because the precipitating injury commonly involves the dermis, which is rich with nerve endings. (more…)
Read MorePros and cons of hydrocolloid dressings for diabetic foot ulcers
Diabetic foot ulcers stem from multiple factors, including peripheral neuropathy, high plantar pressures, decreased vascularity, and impaired wound healing. Contributing significantly to morbidity, they may cause limb loss and death. (See Foot ulcers and diabetes.)
Initially, hydrocolloid dressings were developed to function as part of the stomal flange. Based on their success in protecting peristomal skin, they were introduced gradually into other areas of wound care. They contain wafers of gel-forming polymers, such as gelatin, pectin, and cellulose agents, within a flexible water-resistant outer layer. The wafers absorb wound exudate, forming a gel and creating a moist healing environment. (more…)
Read MoreEmpowering patients to play an active role in pressure ulcer prevention
Developing a pressure ulcer can cause the patient pain, lead to social isolation, result in reduced mobility, and can even be fatal. According to the Agency for Healthcare Research and Quality, estimated costs for each pressure ulcer range from $37,800 to $70,000, and the total annual cost of pressure ulcers in the United States is an estimated $11 billion.
Nurses understand their role in preventing pressure ulcers, but what role do patients play in the prevention plan? Nurses need to empower the patient to be an active member in health promotion activities and participate in prevention measures. In this article, I highlight the importance of incorporating pressure ulcer prevention into patient education for high-risk patients as a way to empower patients. Empowered patients can help improve outcomes and reduce overall costs of this hospital-acquired complication. (more…)
Read MoreRestorative nursing programs help prevent pressure ulcers
Immobility affects all our body systems, including our skin. According to the National Pressure Ulcer Advisory Panel, many contributing factors are associated with the formation of a pressure ulcer, with impaired mobility leading the list.
So what can clinicians do to prevent harm caused by immobility? One often-overlooked strategy is a restorative nursing program. (See About restorative nursing.)
Moving up the time line
Most patients who score poorly for mobility and/or activity impairments on the Braden Scale for Predicting Pressure Ulcer Risk are referred to physical therapy, but too often a restorative nursing program (more…)
Read MoreTime to select a support surface
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
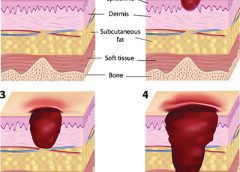
Having the proper support surface for beds and wheelchairs is imperative in preventing pressure ulcers. “Pressure” ulcers are named that for a reason—pressure is the primary cause of interruption of blood flow to the tissue. Unfortunately, guidelines for support surface selection tend to make recommendations for the type of surface to use after a pressure ulcer has developed. Another factor that complicates matters is the development of deep-tissue injuries. These injuries start at the bone level, which means that often, tissue damage is extensive before we see visible signs and realize that the support surface we chose might not have been effective enough. (more…)
Read MoreClinical Notes: Modified Braden Risk Score, dialysis patients, plantar
Modified Braden risk score proposed
A study in Ostomy Wound Management states the risk classification of patients using Braden Scale scores should comprise three (rather than five) levels: high risk, with a total score ≤11; moderate risk, with a total score of 12 to 16; and mild risk, with a total score ≥17.
The retrospective analysis of consecutively admitted patients at risk for pressure ulcer to an acute-care facility included 2,625 patients, with an age range from 1 month to 98 years; 3.1% developed a pressure ulcer. (more…)
Read MoreRole of the ostomy specialist clinician in ileal pouch anal anastomosis surgery
By Leanne Richbourg, MSN, RN, APRN-BC, CWON-AP, CCCN, GCNS-BC
Restorative proctocolectomy with ileal pouch anal anastomosis (IPAA) is the gold standard for surgical treatment of ulcerative colitis (UC) or familial adenomatous polyposis (FAP). It’s also done to treat colon and rectal cancers, such as those caused by Lynch syndrome (LS). IPAA allows the patient to maintain fecal continence and evacuate stool from the anus after colon and rectum removal. A temporary ileostomy may be part of the overall process, but there’s no need for a permanent stoma. (See Understanding ulcerative colitis, FAP, and Lynch syndrome.) (more…)
Read MoreClinician Resources: falls, npuap, patient safety, civility
End your year by checking out these resources for your practice.
Sentinel event alert for falls
As part of its sentinel event alert “Preventing falls and fall-related injuries in health care facilities,” The Joint Commission has assembled information and multiple resources, including:
- analysis of contributing factors for falls
- evidence-based suggestions for improvement
- Joint Commission requirements relevant to falls
- links to toolkits and protocols
- an infographic on preventing falls.
2015 Journal: July – Aug Vol. 4 No. 4
A collaborative approach to wound care and lymphedema therapy: Part 2
By Erin Fazzari, MPT, CLT, CWS, DWC
Have you seen legs like these in your practice?
These legs show lymphedema and chronic wounds before treatment (left image) and after treatment (right image) with complex decongestive therapy (CDT)—the gold standard of lymphedema care. The patient benefited from multidisciplinary collaboration between wound care and lymphedema therapists. (more…)
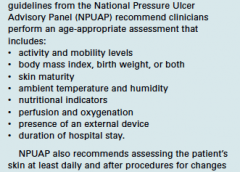
Read MoreComprehensive skin assessment
By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS
Each issue, Apple Bites brings you a tool you can apply in your daily practice. Here’s an overview of performing a comprehensive skin assessment.
In the healthcare setting, a comprehensive skin assessment is a process in which the entire skin of a patient is examined for abnormalities. It requires looking at and touching the skin from head to toe, with a particular emphasis on bony prominences and skin folds. Comprehensive skin assessment is repeated on a regular basis to determine whether changes in the skin’s condition have occurred. The goal of a skin assessment is to identify problem areas promptly for treatment and prevention. (more…)
Read More