Modified Braden risk score proposed
A study in Ostomy Wound Management states the risk classification of patients using Braden Scale scores should comprise three (rather than five) levels: high risk, with a total score ≤11; moderate risk, with a total score of 12 to 16; and mild risk, with a total score ≥17.
The retrospective analysis of consecutively admitted patients at risk for pressure ulcer to an acute-care facility included 2,625 patients, with an age range from 1 month to 98 years; 3.1% developed a pressure ulcer.
The authors of “A retrospective analysis of pressure ulcer incidence and modified Braden Scale score risk classifications” conclude that the modified Braden Scale “may be more convenient and feasible in clinical practice.”
 Amputations and foot-related hospitalization in dialysis patients
Amputations and foot-related hospitalization in dialysis patients
“Amputations and foot-related hospitalisations disproportionately affect dialysis patients,” even though the incidence of foot ulcers is the same in dialysis patients and patients with an ulcer history.
The study in International Wound Journal included 150 consecutive patients with diabetes who were on dialysis and 150 patients with a history of foot ulceration. Each patient was followed for 30 months.
 Plantar shear plays important role in foot ulcers
Plantar shear plays important role in foot ulcers
Considering both plantar shear and pressure, as opposed to pressure alone, is more effective in preventing foot ulcers, according to a study in Diabetes Care.
“Peak plantar shear and pressure and foot ulcer locations: A call to revisit ulceration pathomechanics” notes that pressure is a poor predictor of foot ulcer in patients with diabetes, and pressure-reducing therapeutic footwear has minimal effect in preventing recurrent ulceration.
The authors write that their findings indicate that plantar shear has a “clinically significant role in ulceration” and that ulcers at different sites may have different pathologies. They also call for more research on plantar shear.
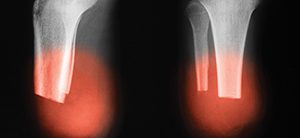
 Lower extremity amputation in patients with diabetes
Lower extremity amputation in patients with diabetes
A longitudinal study in Diabetes Care reports that people with diabetes who have undergone lower-extremity amputation “are more likely to die at any given point in time” compared to those who have not experienced amputation.
“Diabetes, lower-extremity amputation, and death” notes that complications from diabetes account for only some of the variation.
 AHA releases new CPR guidelines
AHA releases new CPR guidelines
The American Heart Association has published the “2015 Guidelines Update for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC)” in the journal Circulation. The guidelines recommend chest compressions at a rate of 100 to 120 per minute and to a depth of at least 2 inches (avoiding depths greater than 2.4 inches). Other recommendations include having clinicians perform steps simultaneously to reduce the time to the first chest compression.
Bystanders should use mobile phones to immediately call 911, placing the phones on speaker, so the dispatcher can offer assistance. Untrained bystanders should provide Hands-Only CPR, and bystanders who are trained in CPR should add breaths in a 30:2 compressions-to-breath ratio.
 Diabetes increases risk of fracture
Diabetes increases risk of fracture
“Type 1 diabetes is associated with an increased risk of fracture across the life span: A population-based cohort study using The Health Improvement Network (THIN)” included patients with and without diabetes, who were matched on parameters such as age and sex.
The risk of fracture was lowest in males and females younger than 20 years and highest in men ages 60 to 69, according to the study, which was published in Diabetes Care. Lower extremity fractures accounted for a higher proportion of incident fractures in participants with diabetes compared to those without. Secondary analyses for incident hip fractures identified the highest hazard ratio of 5.64 in men ages 60 to 69 and the highest hazard ratio of 5.63 in women ages 30 to 39.
 Nurses play important role in quality of life for ostomy patients
Nurses play important role in quality of life for ostomy patients
“Analysing the role of support wear, clothing and accessories in maintaining ostomates’ quality of life,” published in Gastrointestinal Nursing, notes that nurses with expertise in stoma care can help patients with ostomies achieve optimal quality of life by using their expertise to guide patients in making decisions that will help them return to the activities, sports, hobbies, and lifestyle they enjoyed before surgery.
Liposuction may be helpful for lymphedema
“Complete reduction of arm lymphoma following breast cancer—A prospective twenty-one years’ study” concludes that liposuction is effective for treating chronic, nonpitting leg lymphedema in patients who don’t respond to conservative treatment.
The study, published in Plastic and Reconstructive Surgery, included 146 women, with a mean age of 63 and a mean duration of arm swelling of 9 years. It notes that reduced volume is maintained through constant use of compression garments.
DISCLAIMER: All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.