By Roxana Reyna, BSN, RNC-NIC, WCC, CWOCN
As wound care clinicians, we are trained—and expected—to help heal wounds in patients of any age and to achieve positive outcomes. Basic wound-healing principles apply to all patients, whatever their age or size. The specific anatomy and physiology of vulnerable pediatric patients, however, requires detailed wound care. Unfortunately, little evidence-based research exists to support and direct the care of pediatric patients with pressure ulcers. This article describes efforts to reduce pressure ulcers in pediatric patients at Driscoll Children’s Hospital (DCH) in Corpus Christi, Texas.
Making a change
DCH began tracking pressure-ulcer incidence and prevalence in 2010. Data collected by the hospital’s pressure-ulcer prevention specialists showed a high rate of pressure ulcers in the neonatal and pediatric intensive care units. At that time, the hospital lacked a specific pressure-ulcer prevention plan. When it joined the National Database of Nursing Quality Indicators®, leaders decided to create a time-specific measurable goal—to decrease pressure ulcers by 50% within 18 months of implementing a prevention program.
DCH recruited me as their skin-care and wound-prevention specialist to assist the wound care collaborative team in creating the prevention program. The core of the program is a multidisciplinary team approach. Team members include a nursing administrator, physician, certified wound ostomy nurse, wound-care certified nurses, nurse educators, skin-care champions, physical therapist, occupational therapist, dietitian, and representatives of the materials management, environmental services, and case management departments. Called the SKIN team (short for “Saving Kids’ Integument Now”), its motto is “Prevention is critical.” The team involves the patient’s family member or guardian in developing and implementing the plan of care. The pressure-ulcer prevention program includes a bundle of components that have reduced pressure ulcers in adult populations, along with recommendations from the pediatric sections of the 2014 guidelines of the National Pressure Ulcer Advisory Panel (NPUAP).
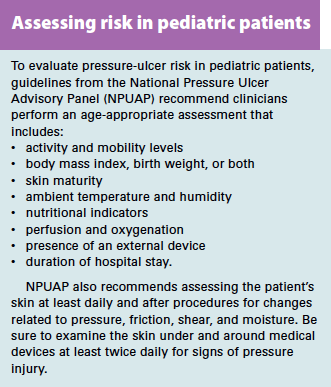
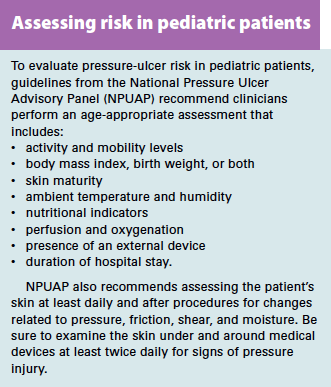
Assessment
As in adults, many factors contribute to skin breakdown and pressure ulcers in pediatric patients—duration and amount of pressure, friction, shear, moisture, perfusion, malnutrition, infection, anemia, and immobility. The 2014 NPUAP guidelines describe risk factors to assess for in pediatric patients. (See Assessing risk in pediatric patients.)
Management
The DCH pressure-ulcer prevention program addresses physician, staff nurse, and nurse-technician education; skin-care regimen; nutritional optimization; appropriate support surfaces and patient repositioning; moisture management; and guidelines for implementing care.
Education
Pressure-ulcer prevention education is a mandatory yearly competency for all nursing and clinical staff. Physicians also receive education on pressure-ulcer staging and proper documentation and coding of pressure ulcers. Quarterly skin-care fairs teach staff about skin- and wound-care products used at DCH, including product selection. Staff can view demonstrations on how to apply these products and learn how to document skin care in the electronic health record. Also, they can get troubleshooting tips on stoma care, gastrostomy-tube sites, and diaper care. Home health agencies are invited to attend the fairs as part of an outreach to promote continuity of care.
Skin-care regimen
DCH has standardized its skin-care line for use with patients ranging from the smallest, most fragile neonates in the neonatal intensive care unit to young adults. Product evaluation on our neonatal patients found no adverse reactions over thousands of applications. The skin-care products we use are made for sensitive skin and contain natural oils and botanicals that provide cleansing, nourishment, and moisture.
Optimizing nutrition
Patients at risk for pressure ulcers require adequate nutrition and hydration; the plan of care must address these needs. Nutritional supplements, including parenteral and enteral supplements, are used as needed to meet children’s nutritional goals.
Appropriate support surfaces
As part of our pressure-ulcer prevention program, we assessed all mattresses and surfaces in warmers, isolettes, cribs, bassinettes, and standard hospital beds. We found the mattresses in our pediatric intensive care unit (PICU) were years older than manufacturers’ recommendations.
In light of the limited sizes available and minimal literature on neonatal and pediatric support surfaces, we asked a company to make prototypes for neonate and infant surfaces. Before finalizing our purchase decision, we conducted a small study to evaluate the pressure redistribution of support surfaces and outcomes by performing pressure mapping on multiple pressure-redistribution surfaces—standard foam, high-resiliency multilayered pressure redistribution foam, and viscoelastic multilayered pressure-redistribution foam. To determine the effectiveness of each surface, we used pressure mapping with an X3 sensor. A comparison of average pressures (mm Hg) found viscoelastic multilayered surfaces provided the greatest pressure redistribution and had lower average interface pressures.
Based on these results, we chose a true pressure-redistribution mattress for our special populations. All PICU mattresses have been upgraded to a nonpowered pressure-redistribution mattress replacement system with self-adjusting technology. Remaining standard beds have been converted to an innovative mattress replacement system. Although the mattresses are made from the best performance materials, repositioning patients every 2 hours and as needed remains an important nursing intervention in preventing pressure ulcers.
Moisture management
DCH replaced cloth pads with disposable underpads manufactured with a new technology that keeps the patient dry by wicking away moisture. Barrier creams are used for the diaper area to help protect skin integrity.
Getting results
Data show that since DCH implemented its pressure-ulcer prevention program, our pressure-ulcer incidence has fallen 66%. These results show pressure ulcers can be prevented by identifying patients at risk and implementing appropriate prevention strategies. At DCH, our ultimate goal is zero hospital-acquired pressure ulcers.
Roxana Reyna is a skin and wound care specialist at Driscoll Children’s Hospital in Corpus Christi, Texas.
Selected references
Brem H, Maggi J, Neirman D, et al. High cost of stage IV pressure ulcers. Am J Surg. 2010;200(4):473-7.
Bryant R, Nix D. Acute and Chronic Wounds: Current Management Concepts. 4th ed. St. Louis, MO: Mosby; 2012.
Delmore B, Lebovits S, Baldock P, Suggs B, Ayello EA. Pressure ulcer prevention program: a journey. J Wound Ostomy Continence Nurs. 2011;38(5):505-13.
Galvin PA, Curley MA. The Braden Q+P: a pediatric perioperative pressure ulcer risk assessment and intervention tool. AORN J. 2012;96(3):261-70.
Hanson D, Thompson P, Langemo D, Hunter S, Anderson J. Pressure mapping: a new path to pressure ulcer prevention. Wound Care Advisor. 2012;1(1):15-9.
How-to Guide: Prevent Pressure Ulcers. Cambridge, MA: Institute for Healthcare Improvement; 2011. www.ihi.org/resources/Pages/Tools/HowtoGuidePreventPressureUlcers.aspx
McCaskey MS, Kirk L, Gerdes C. Preventing skin breakdown in the immobile child in the home care setting. Home Healthc Nurse. 2011;29(4):248-55.
National Pressure Ulcer Advisory Panel, European Pressure Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Emily Haelser, ed. Cambridge Media: Perth, Australia; 2014.
Noonan C, Quigley S, Curley MAQ. Using the Braden Q Scale to predict pressure ulcer risk in pediatric patients. J Pediatr Nurs. 2011;26(6):566-75.
Pieper B, Ratliff C; National Pressure Ulcer Advisory Panel. Registered Nurse Competency-Based Curriculum: Pressure Ulcer Prevention. www.npuap.org/wp-content/uploads/2012/03/NPUAP-RN-Curr-landscape1.pdf
DISCLAIMER: All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.