Case study: Bariatric patient with serious wounds and multiple complications
Despite the healthcare team’s best efforts, not all hospitalizations go smoothly. This article describes the case of an obese patient who underwent bariatric surgery. After a 62-day hospital stay, during which a multidisciplinary team collaborated to deliver the best care possible, he died. Although the outcome certainly wasn’t what we wanted, we’d like to share his story to raise awareness of the challenges of caring for bariatric patients.
An easy tool for tracking pressure ulcer data
By David L. Johnson, NHA, RAC-CT As a senior quality improvement specialist with IPRO, the Quality Improvement Organization for New York State over the past 11 years, I’ve been tasked with helping skilled nursing facilities (SNFs) embrace the process of continuous quality improvement. A necessary component of this effort has been to collect, understand, and analyze timely and accurate data.…
Building an effective pressure ulcer prevention program
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN As a wound care nurse, do you feel the weight of the world on your shoulders when trying to implement a pressure ulcer prevention program? Many staff members think it’s up to the wound care nurse alone to implement the program. However, a successful program requires involvement from all staff and is…
Case study: Bariatric patient with serious wounds and multiple complications
By Hedy Badolato, RD, CSR, CNSC; Denise Dacey, RD, CDE; Kim Stevens, BSN, RN, CCRN; Jen Fox, BSN, RN, CCRN; Connie Johnson, MSN, RN, WCC, LLE, OMS, DAPWCA; Hatim Youssef, DO, FCCP; and Scott Sinner, MD, FACP Despite the healthcare team’s best efforts, not all hospitalizations go smoothly. This article describes the case of an obese patient who underwent bariatric…
Clinical Notes: Radiation & Lymphedema, Decline in Diabetic Foot Ulcers
Radiation and lymphedema Radiation therapy doesn’t increase the incidence of lymphedema in patients with node-negative breast cancer, according to research presented at the American Society for Radiation Oncology’s 56th Annual Meeting held this fall.
Clinician Resources: United Ostomy Association, NGC, NCCN, Experts
Here is a list of valuable ostomy resources, some suggested by our colleagues who follow Wound Care Advisor on Twitter. United Ostomy Association of America The United Ostomy Association of America provides comprehensive resources for patients, including information about the types of ostomies and issues related to nutrition, sexuality, and travel. Much of the information is also available in Spanish…
Developing a successful program for wound care in the home
By Stanley A. Rynkiewicz III, MSN, RN, WCC, DWC, CCS Developing a successful wound care program requires a strong commitment and a willingness to learn. Our experience with creating such a program at Deer Meadows Home Health and Support Services, LLC (DMHHSS), a nonprofit home-care facility in Philadelphia, Pennsylvania, may help others build a similar wound care program and reap…
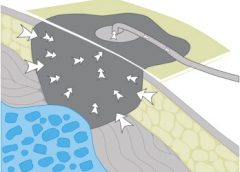
Linear wound measurement basics
By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS Each issue, Apple Bites brings you a tool you can apply in your daily practice. Measurement of wounds is an important component of wound assessment and provides baseline measurements, enables monitoring of healing rates, and helps distinguish among wounds that are static, deteriorating, or improving. All alterations in skin integrity,…
Make your patient-teaching idea a patented reality
By Joy Hooper, BSN, RN, CWOCN, OMS Have you ever had an idea for improving patient care that you wanted to market? You may have lacked confidence or know-how, as I once did. But one patient, a crafty idea, and a trip to Walmart put me on the path to becoming a successful nurse entrepreneur.

Using maggots in wound care: Part 2
By Ronald A. Sherman, MD; Sharon Mendez, RN, CWS; and Catherine McMillan, BA Note From the Editor: This is the second of two articles on maggot therapy. The first article appeared in our July/August 2014 issue, Read part 1 here. Whether your practice is an acute-care setting, a clinic, home care, or elsewhere, maggot debridement therapy (MDT) can prove to…
What to do when someone pushes your buttons
By Laura L. Barry, MBA, MMsc, and Maureen Sirois, MSN, RN, CEN, ANP Why is it that some things don’t bother us, while other things catapult us from an emotional 0 to 60 mph in a heartbeat? We all know what it feels like when someone says or does something that gets our juices flowing. We feel it in our…
When should we take “No” for an answer?
By: Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS Have you ever had a patient yell “Get out of my room!” or “Don’t touch me! I don’t want to be turned”? How about “No! Don’t put those compression stockings on my legs!” or “No, I’m not going to wear those ugly orthopedic shoes!” or “No way. I can’t stay in bed.…
Click here to access the digital edition