The National Pressure Ulcer Advisory Panel (NPUAP) describes support surfaces as “specialized devices for pressure redistribution designed for management of tissue loads, microclimate, and/or other therapeutic functions.” These devices include specialized mattresses, mattress overlays, chair cushions, and pads used on transport stretchers, operating room (OR) tables, examination or procedure tables, and gurneys. Some support surfaces are part of an integrated bed system, which combines the bed frame and support surface into a single unit. (more…)
Read MoreSearch Results for: cms
Knowing when to ask for help
As a wound care expert, you’re probably consulted for every eruption, scrape, and opening in a patient’s skin. Occasionally during a patient assessment, you may scratch your head and ask yourself, “What is this? I’ve never seen anything like it.”
Most wound care experts want to help heal everyone, and most of us love a challenge. But when should we step back and consider referring the patient to another clinician? (more…)
Read MoreOur gold medal issue: Best of the Best 2016
This issue marks the fourth anniversary of the “Best of the Best” issue of Wound Care Advisor, the official journal of the National Alliance of Wound Care and Ostomy. Fittingly, it comes during an Olympics year. Since 1904, the Olympics have awarded gold medals to athletes whose performance makes them the “best of the best.” This year, we’re proud to present our own “Best of the Best” in print format. (more…)
Read More2016 Journal: July – August Vol. 5 No. 4
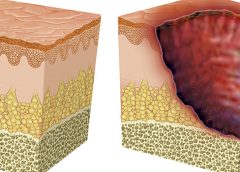
Understanding NPUAP’s updates to pressure ulcer terminology and staging
On April 13, 2016, the National Pressure Ulcer Advisory Panel (NPUAP) announced changes in pressure ulcer terminology and staging definitions. Providers can adapt NPUAP’s changes for their clinical practice and documentation, but it’s important to note that, as of press time, the Centers for Medicare & Medicaid Services (CMS) has not adopted the changes. This means that providers can’t use NPUAP’s updates when completing CMS assessment forms, such as the Minimum Data Set (MDS) or Outcome and Assessment Information Set (OASIS). Instead, they must code the CMS assessment forms according to current CMS instructions and definitions. In addition, there is no ICD-10 code for pressure injury. (more…)
Read MoreDoing it cheaply vs. doing what’s best for patients
Sad but true: Much of what we do as healthcare professionals is based on reimbursement. For nearly all the services and products we use in wound care and ostomy management, Medicare, Medicaid, and insurance companies control reimbursement. For many years, these payers have been deciding which interventions, medications, products, and equipment are the best, and then reimbursing only for those items. If we want to use something not on the list, we—or our patients—will have to pay for it out of pocket. (more…)
Read More2015 Journal: November – December Vol. 4 No. 6
A pressure ulcer by any other name
Just when we think we’ve figured out pressure ulcer staging, it changes again. In April 2016, the National Pressure Ulcer Advisory Panel (NPUAP) held a consensus conference on staging definitions and terminology. The purpose: to analyze and discuss the rationale for the panel’s changes. One of the key changes is replacing the term “pressure ulcer” with “pressure injury.” So instead of calling it a pressure ulcer staging system, NPUAP will refer to it as a pressure injury staging system. The panel explained that the new terminology “more accurately describes pressure injuries to both intact and ulcerated skin.” Other changes include: (more…)
Read MoreCaution: Checklists may lead to inaccurate documentation
Using a checklist form to document wound care can make the task easier and faster—and help ensure that you’ve captured all pertinent data needed for assessment, reimbursement, and legal support. But the form itself may not be comprehensive; some important fields may be missing.
Recently, we at Wound Care Advisor received a question from a clinician who was having trouble deciding how to code a patient’s wound in her hospital’s electronic health record (EHR). Her patient’s specific wound and tissue types weren’t available options in the dropdown menu on the software system. Luckily, on investigating, we discovered her system provided the option to override the checklist and add comments in a notes section. (more…)
Read MoreTop 10 outpatient reimbursement questions
At the 2015 Wild on Wounds conference, the interactive workshop “Are You Ready for an Outpatient Reimbursement Challenge?” featured a lively discussion among participants about 25 real-life reimbursement scenarios. Here are the top 10 questions the attendees asked, with the answers I provided.
Q Why is it necessary for qualified healthcare professionals (QHPs) such as physicians, podiatrists, nurse practitioners, physician assistants, and clinical nurse specialists to identify the place of service where they provide wound care services and to correctly state the place of service on their claim forms? (more…)
Read MoreDon’t go it alone
A fundamental rule of wound care is to treat the “whole” patient, not just the “hole” in the patient. To do this, we need to focus on a holistic
approach to healing, which means evaluating everything that’s going on with the patient—from nutrition, underlying diseases, and medications to activity level, social interactions, and even sleep patterns.
We know that as specialists, we’re expected to do all of these things. But in the real world, we can’t be specialists in all areas. That’s where the team concept comes in. In fact, the team approach is imperative for helping us heal our patients’ wounds and achieve our overall goal of improving patient outcomes. (more…)
Read MoreRestorative nursing programs help prevent pressure ulcers
Immobility affects all our body systems, including our skin. According to the National Pressure Ulcer Advisory Panel, many contributing factors are associated with the formation of a pressure ulcer, with impaired mobility leading the list.
So what can clinicians do to prevent harm caused by immobility? One often-overlooked strategy is a restorative nursing program. (See About restorative nursing.)
Moving up the time line
Most patients who score poorly for mobility and/or activity impairments on the Braden Scale for Predicting Pressure Ulcer Risk are referred to physical therapy, but too often a restorative nursing program (more…)
Read More