By Cheryl Robillard, PT, WCC, CLT, DWC
Patients in your clinical practice who develop wounds should prompt a call for “all hands on deck” to manage the situation, but some personnel may be missing the boat. Physical therapists (PTs), occupational therapists (OTs), and speech-language pathologists (SLPs) should be on board your wound care ship so patients can receive care they need. But unfortunately, sometimes they aren’t.
Several reasons can account for the lack of therapy involvement in some facilities. They include a knowledge deficit of what PTs, OTs, and SLPs can do to help heal wounds, or misinformation such as the myth that therapy can’t get involved until a wound has been present for 30 days. Another reason may be lack of therapist’s knowledge or desire to treat wounds and their complications. Lastly, it could be a “turf” issue when several members of the team could perform a similar intervention.
Let’s take a closer look at some of these areas.
Therapy services
An understanding of the services therapists can provide helps you know when to make referrals.
Cognition assessment
SLPs are experts in assessing a patient’s cognition. The assessment includes learning ability, so they can help the team determine effective strategies for teaching.
Consider the nonadherent patient with diabetes who has a foot wound. Diabetes is a risk factor for cognitive impairment, but how many of your patients with diabetes have been tested for this impairment so they—and you—know how to compensate?
Another problem is that patients with mild cognitive impairment can often “talk the talk, but not walk the walk”: They may say they understand but not truly “get it.” This is especially true with written information. Too much money has been wasted on literature given to patients who might be able to read it but don’t comprehend the information or can’t make the connection between the information and what specifically they need to do.
You can use a simple screening test such as the SLUMS (St. Louis University Mental Status exam) or the MoCA (Montreal Cognitive Assessment) for an initial assessment and refer patients to an SLP if the results are positive.
Nutrition
SLPs and OTs, working closely with dietitians, can assess and treat swallowing and feeding issues that can impair the ability of patients to receive the nutrition they need for wound healing. SLPs and OTs also can educate staff and patients in good oral care to help prevent such complications as pneumonia that can derail healing.
Skin care
General skin care isn’t only the function of nursing—OTs and PTs can help. Ensuring that patients and caregivers have the knowledge and capability to inspect, cleanse, and moisturize the skin should be part of a complete activities-of-daily-living program, a specialty of OTs.
Urinary and bowel continence management, which is within the scope of practice for PTs and OTs, can make a significant difference in avoiding contamination of truncal wounds.
Pressure reduction and off-loading is another reason for referral to PTs and OTs. Splinting and contracture management can prevent some wounds and help in healing others. PTs can assess sensation and examine footwear, then teach patients and make recommendations to prevent excessive pressure. They also can provide specialty shoes or total contact casts. Decisions about pressure redistribution in seating systems and beds should involve PTs or OTs.
Edema management
Edema management, which may include manual lymphatic drainage, compression, and exercise, is a good reason to refer patients to PTs and OTs. Although some of these methods require additional training beyond entry-level education, therapists should be able to provide them.
Psychosocial issues
OTs also address psychosocial issues pertinent to wound healing. For example, a patient confined to bed or home for extended periods of time may experience social isolation, learned helplessness, and depression. A patient with a vascular wound who is at risk for amputation may experience extreme stress. Or a patient may not be able to return to his or her previous profession because of wound issues. OTs are trained to provide psychotherapeutic interventions aimed at improving and maintaining the highest quality of life.
Debridement
Debridement of nonviable tissue, including both necrotic tissue and epiboly, is part of clinical practice for PTs and specially trained OTs. These therapists can use scalpels, forceps, curettes, and scissors for conservative sharp debridement. Sterile instruments are used in a clean environment to remove only nonviable tissue. This differs from surgical debridement, which is completed by physicians in a sterile surgical environment and may also include removal of viable tissue to effectively create a new wound. Debridement may also be nonspecific, such as using pulsed lavage, a high-pressure saline jet with suction.
Please note that all of the interventions discussed so far may be provided when needed, regardless of the length of time a wound has been present.
Biophysical agents
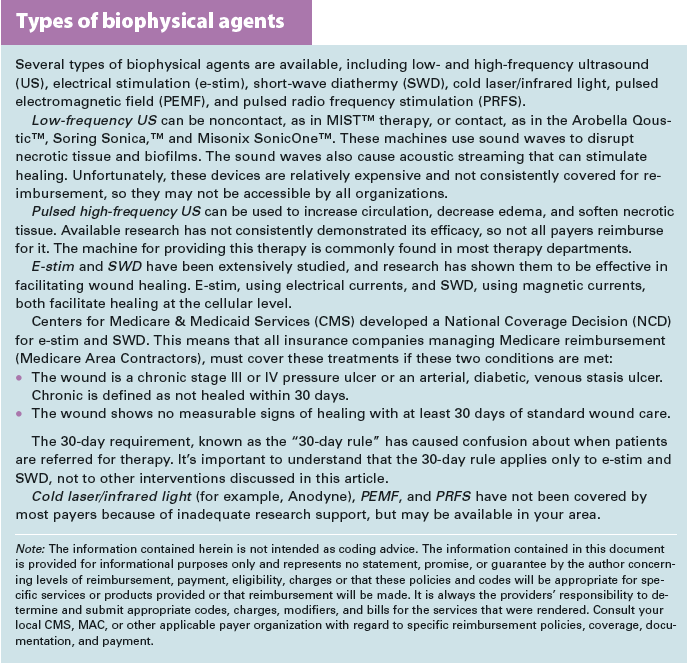
Biophysical agents, also commonly known as modalities, use various forms of energy to facilitate healing by decreasing inflammation, increasing circulation, decreasing edema, decreasing pain, and removing or softening necrotic tissue. PTs and specially trained OTs can provide these modalities. Each modality has specific contraindications and may have payer-specific limitations on provision. (See Types of biophysical agents.)
Bringing therapists onboard
Now that you know what therapists should be able to do for your wound patients, what if your clinicians aren’t trained in some of these areas? Discuss the problem with the department manager because there are many continuing education courses available, as well as the Wound Care Education Institute certification program.
An excellent way to increase involvement of therapists in wound care is to have them participate in wound rounds with nurses. This is a great way for you to share your knowledge with them, allow them to see various wounds and wound dressings, and have them determine with you what wounds might need the therapy interventions discussed in this article.
Mowing down turf issues
Eliminating turf issues begins with knowing each discipline’s scope of practice. You also may need to take financial issues into consideration. Depending on your setting, if the PT can debride and be separately reimbursed, freeing up nurses to focus on other medical issues, wouldn’t that be the most expedient course?
Another potential problem may be coordination of services. For example, although applying a dressing is not a billable therapy service, does it make sense to have a therapist undress the wound for a modality then leave the wound uncovered until a nurse has time to apply the dressing?
Resolving turf issues requires a collaborative spirit from all team members to negotiate what makes the most sense in your setting and determine what would be best for the patient’s healing.
Setting sail
Having therapists as active members of your wound care team will ensure you’re providing the best state-of-the-art care for patients’ wounds. Knowing what the different therapies can do will help you determine which wounds require a therapist’s direct involvement. Lastly, navigating barriers to getting your therapists on board your wound care ship will help you reach top speed in sailing to healing!
Selected references
Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: A meta analysis of longitudinal studies. Intern Med J. 2012;42(5):484-91.
McCrimmon RJ, Ryan CM, Frier BM. Diabetes 2: diabetes and cognitive dysfunction. Lancet. 2012;379:
2291-2299.
Marseglia A, Xu W, Rizzuto D, et al. Cognitive functioning among patients with diabetic foot. J Diabetes Complications. 2014;28(6):863-868.
Nasreddine ZS, Phillips NA, Bedirian V, et al The Montreal Cognitive Assessment, MoCa: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695-9.
Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 2010;25(1):61-8.
Tariq SH, Tumosa N, Chibnall JT, et al. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder—a pilot study. Am J Geriatr Psychiatry. 2006;14(11):900-10.
Whitmer RA. Type 2 diabetes and risk of cognitive impairment and dementia. Curr Neurol Neurosci Rep. 2007;7(5):373-80.
Cheryl Robillard is a clinical specialist for Aegis Therapies in Milwaukee, Wisconsin.
DISCLAIMER: All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.