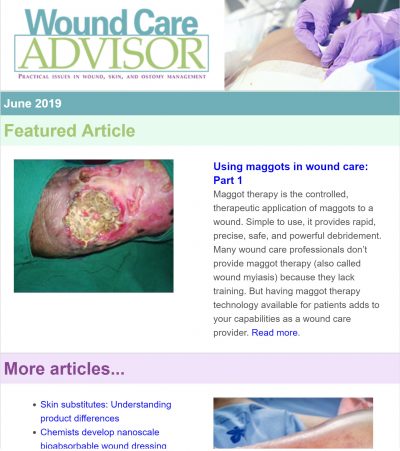
Using maggots to treat wounds dates back to 1931 in this country. Until the advent of antibiotics in the 1940s, maggots were used routinely. In the 1980s, interest in them revived due to the increasing emergence of antibiotic-resistant bacteria.
At Select Specialty Hospital Houston in Texas, we recently decided to try maggot therapy for a patient with a particularly difficult wound. In this case study, we share our experience. (more…)
Read More
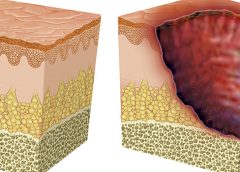
As full-thickness wounds heal, they begin to fill in from the bottom upward with granulation tissue. At the same time, wound edges contract and pull together, with movement of epithelial tissue toward the center of the wound (contraction). These epithelial cells, arising from either the wound margins or residual dermal epithelial appendages within the wound bed, begin to migrate in leapfrog or train fashion across the wound bed. Horizontal movement stops when cells meet (contact inhibition). The ideal wound edge is attached to and flush with the wound bed, moist and open with the epithelial rim thin, and pale pink to translucent. (more…)
Read More
Moldable skin barrier effective for elderly patients with ostomy
A study in Gastroenterology Nursing reports that compared to a conventional skin barrier, a moldable skin barrier significantly improves self-care satisfaction scores in elderly patients who have a stoma. The moldable skin barrier also caused less irritant dermatitis and the costs for leakage-proof cream were lower.
“The application of a moldable skin barrier in the self-care of elderly ostomy patients” included 104 patients ages 65 to 79 who had a colostomy because of colorectal cancer.
Risk factors for severe hypoglycemia in older adults with diabetes identified
(more…)
Read More
Just when we think we’ve figured out pressure ulcer staging, it changes again. In April 2016, the National Pressure Ulcer Advisory Panel (NPUAP) held a consensus conference on staging definitions and terminology. The purpose: to analyze and discuss the rationale for the panel’s changes. One of the key changes is replacing the term “pressure ulcer” with “pressure injury.” So instead of calling it a pressure ulcer staging system, NPUAP will refer to it as a pressure injury staging system. The panel explained that the new terminology “more accurately describes pressure injuries to both intact and ulcerated skin.” Other changes include: (more…)
Read More
Wound Care Advisor is owned and published by HealthCom Media. Wound Care Advisor is peer reviewed. The views and opinions expressed in the editorial and advertising material on this website are those of the authors and advertisers and do not necessarily reflect the opinions or recommendations of the NAWCO, the Editorial Advisory Board members, or the Publisher, Editors and staff of Wound Care Advisor.
Wound Care Advisor attempts to select authorities who are knowledgeable in their fields. However, it does not warrant the expertise of any author, nor is it responsible for any statements made by any author. Certain statements about the uses, dosages, efficacy and characteristics of some drugs mentioned here reflect the opinions or investigational experience of the authors. Nurses should not use any procedures, medications, or other courses of diagnosis or treatment discussed or suggested by authors without evaluating the patient’s conditions and possible contraindications or dangers in use, reviewing any applicable manufacturer’s prescribing or usage information, and comparing these with recommendations of other authorities.
We encourage people with wounds and ostomy questions to contact their care provider; we are unable to provide medical advice.
Read More
Optimizing nutritional status is a key strategy both in preventing and managing pressure ulcers. In patients across all care settings, compromised nutrition— as from poor intake, undesired weight loss, and malnutrition—increases the risk of pressure ulcers. It contributes to altered immune function, impaired collagen synthesis, and decreased tensile strength. In many cases, malnutrition also contributes to wound chronicity and increases the risk for delayed and impaired wound healing. In patients with chronic wounds, such as pressure ulcers, a chronic inflammatory state can induce catabolic metabolism, malnutrition, and dehydration. (more…)
Read More
Topical application of silver nitrate is often used in wound care to help remove and debride hypergranulation tissue or calloused rolled edges in wounds or ulcerations. It’s also an effective agent to cauterize bleeding in wounds. Silver nitrate is a highly caustic material, so it must be used with caution to prevent damage to healthy tissues. (more…)
Read More
Using a checklist form to document wound care can make the task easier and faster—and help ensure that you’ve captured all pertinent data needed for assessment, reimbursement, and legal support. But the form itself may not be comprehensive; some important fields may be missing.
Recently, we at Wound Care Advisor received a question from a clinician who was having trouble deciding how to code a patient’s wound in her hospital’s electronic health record (EHR). Her patient’s specific wound and tissue types weren’t available options in the dropdown menu on the software system. Luckily, on investigating, we discovered her system provided the option to override the checklist and add comments in a notes section. (more…)
Read More
Keeping clinicians up-to-date on clinical knowledge is one of the main goals of the Wild on Wounds (WOW) conference held each September in Las Vegas. Every year, I present the opening session, called “The Buzz Report,” which focuses on the latest-breaking wound care news—what’s new, what’s now, and what’s coming up. I discuss new products, practice guidelines, resources, and tools from the last 12 months in skin, wound, and ostomy management.
In the January issue, I discussed some of the updates from my 2015 Buzz Report. Now I’d like to share a few more, along with some of my favorite resources. (more…)
Read More