BY: NANCY MORGAN, RN, BSN, MBA, WOCN, WCC, CWCMS, DWC
You’ve identified your patient’s lower extremity ulcer as a venous ulcer. It has irregular edges, a ruddy wound base, and a moderate amount of drainage. The patient’s bilateral lower extremities are edematous. As a wound care clinician, you know sustained graduated compression is key to healing stasis ulcers and preventing their recurrence. (more…)
Search Results for: Arte
Wound care treatment explained at Rotary
When treating people for wounds, the care team preforms both a comprehensive diagnosis and comprehensive treatment, Kathy Khandaker, director of wound care at Community Hospitals and Wellness Centers-Bryan, told the Bryan Rotary Club at its Friday meeting.
The wound care clinic opened at CHWC in 2006, added ostomy care in 2007, continence care in 2010 and added a full-time physician in 2015. The care team includes a wound care nurse, a hyperbaric oxygen therapy technician and a receptionist in addition to the physician. (more…)
Read MoreStem Cell Dynamic Therapy Could Heal Wounds
It’s necessary for the skin to heal the wounds after getting injured. For the first time, scientists discovered that the changing stem cell dynamics contribute to wound healing. The main purpose of these studies was to understand how stem cells differentiate, migrate, and proliferate to repair the tissue damage after trauma.
A team from Université libre de Bruxelles (ULB) started their research on stem cells. Professor of ULB, Dr. Cédric Blanpain MD/Ph.D, WELBIO investigator and the lead researcher of this study, defined the cellular and molecular mechanisms that play active roles in wound healing. The research report was first published in the Journal of Nature Communications.
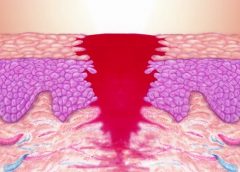
The skin of a creature is just like an outer shield which protects the inner tissues and other organs from outer injuries. If somehow the outer shield gets disrupted then body activates a cascade of cellular and molecular event to repair the damage and restore skin integrity. ScienceDaily reported that minor defects in these events lead to improper repair causing acute and chronic wound disorders.
In the new study, scientists revealed that distinct stem cells populations contribute in healing the wound. Although it is not cleared yet how proliferation, differentiation, and migration get balanced by stem cell populations during the healing process. Co-author of this study Dr.Sophie Dekoninck said in a statement,“The molecular characterization of the migrating leading edge suggests that these cells are protecting the stem cells from the infection and mechanical stress allowing a harmonious healing process”.
Read more at The Science Times
Read MoreReduction of 50% in Diabetic Foot Ulcers With Stem Cells
MUNICH — Local injection of mesenchymal stem cells derived from autologous bone marrow shows promise in healing recalcitrant neuropathic diabetic foot ulcers, a novel study from Egypt shows.
Presenting the results at the European Association for the Study of Diabetes (EASD) 2016 Annual Meeting, Ahmed Albehairy, MD, from Mansoura University, Egypt, said: “In patients who received the mesenchymal stem cells, ulcer reduction was found to be significantly higher compared with patients on conventional treatment after both 6 weeks and 12 weeks of follow-up. This is despite the fact that initial ulcer size was larger in the stem-cell–treated group.” (more…)
Read MoreKnowing when to ask for help
As a wound care expert, you’re probably consulted for every eruption, scrape, and opening in a patient’s skin. Occasionally during a patient assessment, you may scratch your head and ask yourself, “What is this? I’ve never seen anything like it.”
Most wound care experts want to help heal everyone, and most of us love a challenge. But when should we step back and consider referring the patient to another clinician? (more…)
Read MoreLymphedema and lipedema: What every wound care clinician should know
Imagine you have a health condition that affects your life every day. Then imagine being told nothing can be done about it; you’ll just have to live with it. Or worse yet, your physician tells you the problem is “you’re just fat.”
Many people with lymphedema or lipedema have no idea their condition has a name or that many other people suffer from the same thing. Although lymphedema and lipedema can’t be cured, proper management and resources can help patients cope. This article improves your grasp of these conditions, describes how to recognize and manage them, and explains how to support your patients.
To understand lymphedema and lipedema, first you need to understand how the lymphatic system functions. It makes lymph, then moves it from tissues to the bloodstream. It also plays a major role in the immune system, aiding immune defense. In addition, it helps maintain normal fluid balance by promoting fluid movement from the interstitial tissues back to the venous circulation. (See Lymphatic system: Four major functions.)
If the lymphatic system is impaired from a primary (hereditary or congenital) condition or a secondary problem, lymphedema can result. In this chronic, potentially progressive, and incurable condition, protein-rich fluid accumulates in the interstitial tissues.
Lymphedema basics
Lymphedema occurs in four stages.
Stage 0. During this stage (also called the subclinical or latency stage), transport capacity of the lymphatic system decreases but remains sufficient to manage normal lymphatic loads. Signs and symptomsaren’t evident and can be measured only by sensitive instruments, such as bioimpedance spectroscopy and optoelectronic volumetry. Without such instruments to quantify volume changes, diagnosis may rest on subjective complaints.
In this stage, limited functional reserve of the lymphatic system leads to a fragile balance between subnormal transport capacity and lymphatic loads. Added stress on the lymphatic system (as from extended heat or cold exposure, injury, or infection) may cause progression to stage 1.
Providing appropriate patient information and education, especially after surgery, can dramatically reduce the risk that lymphedema will progress to a more serious stage.
Stage 1. Considered the spontaneously reversible stage, stage 1 is marked by softtissue pliability without fibrotic changes. Pitting can be induced easily. In early stage 1, limb swelling may recede over – night. With proper management, the patient can expect the extremity to decrease to a normal size compared to that of the uninvolved limb. Otherwise, lymphedema is likely to progress to stage 2.
Stage 1 lymphedema may be hard to distinguish from edemas from other causes. Clinicians must rely on the patient history and monitor for swelling resolution with conventional management, such as compression and elevation, or note if swelling persists despite these standard interventions.
Stage 2. Sometimes called the spontaneously irreversible stage, stage 2 is identified mainly from tissue proliferation and subsequent fibrosis (called lymphostatic fibrosis). The fluid component can be removed spontaneously, but removal of the increased tissue proliferation (initially irreversible) takes more time. Tissue proliferation stems from long-standing accumulation of protein-rich fluid; over time, the tissue hardens and pitting is hard to induce. In many cases, swelling volume increases, exacerbating the already compromised local immune defense.
Consequently, infections (particularly cellulitis) are common; these, in turn, increase the volume of the affected area. Proper treatment can reduce volume.
With proper care (complete decongestive therapy [CDT]), lymphedema can stabilize during stage 2. But patients with chronic or recurrent infections are likely to progress to stage 3.
Stage 3. Also called lymphostatic elephantiasis, this stage is marked by further fluid volume increases and progression of tissue changes. Lymphostatic fibrosis becomes firmer and other skin alterations may occur, including papillomas, cysts, fistulas, hyperkeratosis, fungal infections, and ulcers. Pitting may be present. Natural skinfolds deepen (especially those of the dorsum of the wrist or ankle) and, in many cases, cellulitis recurs.
If lymphedema management starts during this stage, reduction can still occur. Even in extreme cases, with proper care and patient adherence to treatment, lymphostatic elephantiasis can be reduced so the leg is a normal or near-normal size.
Assessment and diagnosis
A thorough physical examination is the gold standard for diagnosing lymphedema. A complete patient history, body-systems review, inspection, and palpation can help determine if edema is lymphedema.
Clinically, the only test with proven reliability and validity in diagnosing lymphedema is the Stemmer sign. Fibrotic changes associated with lymphedema can lead to thickened skin over the proximal phalanges of the toes or fingers. If you can’t tent or pinch the skin on the involved extremity, lymphedema is present (a positive Stemmer sign). However, a negative finding (soft, pliable tissue) doesn’t rule out lymphedema because the condition may be in an early stage, before tissue proliferation and fibrosis have set in.
Management
Although incurable, lymphedema can be managed successfully through CDT. This approach involves proper identification of lymphedema, manual lymph drainage, skin and nail care, patient education, compression, and exercise.
CDT has two phases:
• Phase I, the intensive phase, continues until the extremity has decongested or reached a plateau. The clinician provides treatments and educates the patient about all aspects of CDT to prepare him or her for phase II. Phase I can last several weeks to several months depending on lymphedema severity.
• Phase II, the maintenance phase, begins once the extremity has decongested or plateaued. This phase still focuses on CDT, but now the patient, not the clinician, is responsible for all care. The goal is to reduce limb size while enabling the patient to become self-sufficient in managing lymphedema. Although CDT can bring significant improvements in limb size, skin quality, and function, patients must remember that phase II continues lifelong. Be sure to provide education about ongoing self-management strategies.
Lipedema: The disease they call “fat”
Lipedema is a painful disorder of fat deposition. Pathologic deposition of fatty tissue (usually below the waist) leads to progressive leg enlargement. Like lymphedema, lipedema is incurable but manageable. Unless managed properly, lipedema can reduce mobility, interfere with activities of daily living, and lead to secondary lymphedema. (See Lipedema stages.)
Lipedema commonly is misdiagnosed as lymphedema. However, lymphedema involves protein-rich fluid, whereas lip edema is a genetically mediated fat disorder. Because lipedema resists diet and exercise, it can lead to psychosocial complications. Lipedema occurs almost exclusively in women; typically, onset occurs between puberty and age 30. One unpublished epidemiologic study puts lip edema incidence in females at 11%. Some patients have a combination of lipedema and lymphedema. (See Viewing lipolymphedema.)
Assessment and diagnosis
As with lymphedema, lipedema diagnosis rests on clinical presentation. Lipedema characteristics include bilateral and symmetrical involvement, absence of pitting (because lipedema isn’t a fluid disorder), soft and pliable skin, and filling of the retromalleolar sulcus (called the fat pad sign.)
Key signs and symptoms include:
• feeling of heaviness in the legs (aching dysesthesia)
• easy bruising
• sensitivity to touch (called “painful fat syndrome”)
• orthostatic edema
• oatmeal-like changes to skin texture.
Nearly half of lipedema patients are overweight or obese, but many appear of normal weight from the waist up. Essentially, the upper and lower extremities don’t match. The lower extremities typically show fatty deposits extending from the iliac crest to the ankles, sparing the feet. (See Lipedema patterns.)
Management
Lipedema is best managed through weight control, as additional weight gain through adipose tissue tends to deposit in the legs. For patients with concomitant lymphedema (lipolymphedema), modified CDT helps reduce and manage lymphatic compromise. To address excess fat deposition, newer “wet” liposuction techniques have proven beneficial. These techniques gently detach adipose cells from the tissue, helping to preserve connective tissue and lymphatic vessels.
Know what to look for
In both lymphedema and lipedema, early identification and proper diagnosis are key. (See Differentiating lymphedema and lipedema.) A thorough history and physical exam will likely lead to an accurate diagnosis, if clinicians know what to look for. Proper diagnosis and treatment can prevent expensive and ineffective interventions, which can negatively affect both the patient’s condition and psychological well being.
Heather Hettrick is an associate professor at Nova Southeastern University, Department of Physical Therapy in Fort Lauderdale, Florida.
Selected references
Fat Disorders Research Society. Lipedema description.
Fife CE, Maus EA, Carter MJ. Lipedema: a frequently misdiagnosed and misunderstood fatty deposition syndrome. Adv Skin Wound Care. 2010;23(2):81-92
Herbst KL. Rare adipose disorders (RADS) masquerading as obesity. Acta Pharmacol Sin. 2012;33(2):155-72.
National Lymphedema Network. Position papers.
Schmeller W, Hueppe M, Meier-Vollrath I. Tumescent liposuction in lipoedema yields good long-term results. Br J Dermatol. 2012;166(1):161-8.
Zuther J. A closer look at lipedema and the effects on the lymphatic system. December 13, 2012. lymphedemablog.com/2012/12/13/a-closer-look-at-lipedema-and-the-effects-on-the-lymphatic-system/
Zuther J. Stages of lymphedema. October 3, 2012.
Read MorePracticing emotional intelligence may help reduce lateral violence
It’s been a stressful day at work—nothing new. One confused patient pulled off her ostomy bag, you’re having difficulties applying negative-pressure wound therapy on another, and a third patient’s family is
angry with you. We all experience stressful days, but unfortunately, sometimes we take our stress out on each other. Too often, this ineffective way of identifying and managing stress leads nurses to engage in lateral violence. (more…)
Read MoreInstill instead: Negative pressure wound therapy with instillation for complex wounds
Negative pressure wound therapy (NPWT) uses negative pressure to draw wound edges together, remove edema and infectious material, and promote perfusion and granulation tissue development. The tissue stretch and compression created by negative pressure during NPWT promotes tissue perfusion and granulation tissue development through angiogenesis, cellular proliferation, fibroblast migration, increased production of wound healing proteins, and reduction of wound area. NPWT has been used to improve healing in a variety of wounds, including traumatic injuries, surgical wounds, pressure ulcers, diabetic foot ulcers, and venous stasis ulcers. (more…)
Read MoreCase study: Maggots help heal a difficult wound
Using maggots to treat wounds dates back to 1931 in this country. Until the advent of antibiotics in the 1940s, maggots were used routinely. In the 1980s, interest in them revived due to the increasing emergence of antibiotic-resistant bacteria.
At Select Specialty Hospital Houston in Texas, we recently decided to try maggot therapy for a patient with a particularly difficult wound. In this case study, we share our experience. (more…)
Read MorePrivacy Policy
We may use the information we collect from you when you register, make a purchase, sign up for our newsletter, respond to a survey or marketing communication, surf the website, or use certain other site features in the following ways:
Our website is scanned on a regular basis for security holes and known vulnerabilities in order to make your visit to our site as safe as possible.
We use regular Malware Scanning.
We do not sell, trade, or otherwise transfer to outside parties your Personally Identifiable Information unless we provide users with advance notice. This does not include website hosting partners and other parties who assist us in operating our website, conducting our business, or serving our users, so long as those parties agree to keep this information confidential. We may also release information when it’s release is appropriate to comply with the law, enforce our site policies, or protect ours or others’ rights, property or safety.
However, non-personally identifiable visitor information may be provided to other parties for marketing, advertising, or other uses.
Google’s advertising requirements can be summed up by Google’s Advertising Principles. They are put in place to provide a positive experience for users. https://support.google.com/adwordspolicy/answer/1316548?hl=en
Users can set preferences for how Google advertises to you using the Google Ad Settings page. Alternatively, you can opt out by visiting the Network Advertising Initiative Opt Out page or by using the Google Analytics Opt Out Browser add on.
When it comes to the collection of personal information from children under the age of 13 years old, the Children’s Online Privacy Protection Act (COPPA) puts parents in control. The Federal Trade Commission, United States’ consumer protection agency, enforces the COPPA Rule, which spells out what operators of websites and online services must do to protect children’s privacy and safety online.
The Fair Information Practices Principles form the backbone of privacy law in the United States and the concepts they include have played a significant role in the development of data protection laws around the globe. Understanding the Fair Information Practice Principles and how they should be implemented is critical to comply with the various privacy laws that protect personal information.
The CAN-SPAM Act is a law that sets the rules for commercial email, establishes requirements for commercial messages, gives recipients the right to have emails stopped from being sent to them, and spells out tough penalties for violations.
If at any time you would like to unsubscribe from receiving future emails, you can email us at
and we will promptly remove you from ALL correspondence.
If there are any questions regarding this privacy policy, you may contact us using the information below.
Doylestown, PA 18901
How to apply silver nitrate
Topical application of silver nitrate is often used in wound care to help remove and debride hypergranulation tissue or calloused rolled edges in wounds or ulcerations. It’s also an effective agent to cauterize bleeding in wounds. Silver nitrate is a highly caustic material, so it must be used with caution to prevent damage to healthy tissues. (more…)
Read MoreClinical Notes: ostomy, pressure ulcer, burn treatment
Self-management ostomy program improves HRQOL
A five-session ostomy self-care program with a curriculum based on the Chronic Care Model can improve health-related quality of life (HRQOL), according to a study in Psycho-Oncology.
“A chronic care ostomy self-management program for cancer survivors” describes results from a longitudinal pilot study of 38 people. Participants reported sustained improvements in patient activation, self-efficacy, total HRQOL, and physical and social well-being. Most patients had a history of rectal cancer (60.5%) or bladder cancer (28.9%). (more…)
Read More