http://www.sciencedaily.com/releases/2014/07/140715141357.htm
Read MoreSearch Results for: How
How to love and care for yourself unconditionally
By Yolanda G. Smith, MSN, RN, CCRN
Are you able to relax, have fun, and enjoy the simple pleasures of life? Or do you:
- have trouble falling or staying asleep?
- smoke, drink, or eat to reduce tension?
- have headaches, back pain, or stomach problems?
- get irritated or upset over insignificant things?
- have too much to do and too little time to do it?
Bacteria living on skin may affect how wounds heal
How to assess wound exudate
By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS
Each issue, Apple Bites brings you a tool you can apply in your daily practice.
Exudate (drainage), a liquid produced by the body in response to tissue damage, is present in wounds as they heal. It consists of fluid that has leaked out of blood vessels and closely resembles blood plasma. Exudate can result also from conditions that cause edema, such as inflammation, immobility, limb dependence, and venous and lymphatic insufficiency.
(more…)
“This is how we’ve always done it” isn’t good enough
Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Have you ever faced responsibility for a patient-care situation you learned about in school but had yet to encounter in the real world? With so many different health conditions and constant advancements in medical care, it’s not surprising that this happens frequently to many clinicians.
The first and easiest way for most of us to handle this situation is to ask our coworkers what to do. While this isn’t necessarily a bad thing, we as clinicians should reach a little further and get corroboration of what coworkers tell us. What we learn on the job may sound—and even seem—credible but it also needs validity so it can stand up in a legal situation. Recently, I was teaching a class to clinicians on ostomy care when one student shrieked, “Our entire hospital system has been doing this wrong for years.” (more…)
Read MoreHow to apply a spiral wrap
By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS
Each issue, Apple Bites brings you a tool you can apply in your daily practice.
Description
The spiral wrap is a technique used for applying compression bandaging.
Procedure
Here’s how to apply a spiral wrap to the lower leg. Please note that commercial compression wraps come with specific instructions for proper bandaging technique. Be sure to follow these instructions to provide safe and effective compression. (more…)
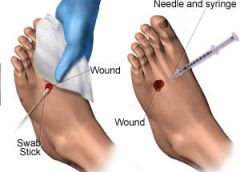
Read MoreWhen and how to culture a chronic wound
By Marcia Spear, DNP, ACNP-BC, CWS, CPSN
Chronic wound infections are a significant healthcare burden, contributing to increased morbidity and mortality, prolonged hospitalization, limb loss, and higher medical costs. What’s more, they pose a potential sepsis risk for patients. For wound care providers, the goal is to eliminate the infection before these consequences arise.
Most chronic wounds are colonized by polymicrobial aerobic-anaerobic microflora. However, practitioners continue to debate whether wound cultures are relevant. Typically, chronic wounds aren’t cultured unless the patient has signs and symptoms of infection, which vary depending on whether the wound is acute or chronic. (See Differentiating acute and chronic wounds.) (more…)
Read MoreHow do you prove a wound was unavoidable?
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
A pressure ulcer that a patient acquires in your facility or a patient’s existing pressure ulcer that worsens puts your organization at risk for regulatory citations as well as litigation. Unless you can prove the pressure ulcer was unavoidable, you could find yourself burdened with citations or fines, or could even end up in court. (more…)
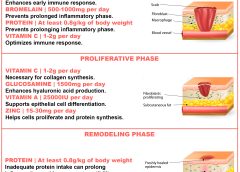
Read MoreHow dietary protein intake promotes wound healing
By Nancy Collins, PhD, RD, LD/N, FAPWCA, and Allison Schnitzer
Nutrition is a critical factor in the wound healing process, with adequate protein intake essential to the successful healing of a wound. Patients with both chronic and acute wounds, such as postsurgical wounds or pressure ulcers, require an increased amount of protein to ensure complete and timely healing of their wounds.
Elderly patients with wounds pose a special challenge because of their decreased lean body mass and the likelihood of chronic illnesses and insufficient dietary protein intake. To promote a full recovery, wound care clinicians must address the increased protein needs of wound patients, especially elderly patients. (more…)
Read MoreHow to fit in fast at your new job
By Gregory S. Kopp, RN, MN, MHA
A new job can be stimulating, but it can also be stressful. Not only will you have new responsibilities, but you’ll also have a new setting, new leaders, and new colleagues. And the quicker you can figure out who’s who and what’s what—without stepping on anyone’s toes—the better off you’ll be.
But establishing positive relationships while performing your new job well can be tricky. And early missteps can have a lasting effect on your working relationships and your effectiveness. That’s why I recommend using the four tactics below, starting on day one. (more…)
Read MoreHow to set up an effective wound care formulary and guideline
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
Navigating through the thousands of wound care products can be overwhelming and confusing. I suspect that if you checked your supply rooms and treatment carts today, you would find stacks of unused products. You also would probably find that many products were past their expiration dates and that you have duplicate products in the same category, but with different brand names. Many clinicians order a product by brand name, not realizing that plenty of the product is already in stock under a different brand name. (more…)
Read MoreHow to keep your communications professional
By Kathleen D. Pagana, PhD, RN
As clinicians, we’re proud of the expert care we provide patients. But we also know that just doing our job isn’t enough to advance our careers. Mastering good communication skills is essential for all clinicians at all career stages—especially with today’s flatter organizational structures and more participatory management styles. Knowing how to communicate in a professional manner can give you the edge you need for career advancement.
Opportunity rarely knocks any more. Instead it may present as a phone call, voice mail, e-mail, or text message. Be sure to use proper etiquette with all communication forms.
Speaking with managers
When dealing with your manager, use a solution-focused approach. Don’t be a complainer. Some communication experts point out that people complain about things they can do something about—not things they have no power over. For example, they don’t complain about their foot size because there’s nothing they can do about it. Yet people often complain about their jobs because they’re unwilling to take the risk of making a change.
We need to take charge of our lives. We can accept the fact—without complaining—that we’re making the choice to stay where we are. Or we can make a request or take action to achieve a desired outcome. Suppose you work on a clinical unit and disagree with the way your manager makes clinical assignments. You have several options:
- Complain to coworkers and make the workplace miserable for others.
- Speak with your manager and make suggestions for improvement.
- Leave your job and go elsewhere if you can’t work with your manager to make things better.
If you decide to stay in your job, accept the fact that you’ve made that choice. Take responsibility for it and stop complaining.
Speaking on the phone with physicians
For clinicians who are not physicians, the key to effective communication with physicians is to remember you’re an important member of the healthcare team. An effective way to guide your communication with physicians and other colleagues is to use a tool such as SBAR (Situation, Background, Assessment, Recommendation). Say, for instance, you want to suggest the doctor order an anxiolytic for your patient. Here’s how you might do it using SBAR:
Situation: “Mrs. Smith is complaining of severe anxiety.”
Background: “She is 1 day post-op from a lumbar laminectomy.”
Assessment: “She is alert and oriented and her vital signs are stable. She has no numbness or tingling in her extremities.”
Recommendation: “She said she takes lorazepam 2 mg orally at when she’s anxious. Would you like to order something for her?”
Before ending the conversation, repeat and clarify the medication order (if the doctor gives one).
Telephone
The sound of your voice and your manners are essential components of phone etiquette. Smile—the smile on your face comes through in your voice. Here are five more tips:
- Get yourself organized before placing the call.
- Minimize background noise.
- Immediately identify yourself. Don’t assume the recipient will recognize your voice.
- Concentrate on listening and avoid multitasking.
- Schedule phone conversations to avoid playing phone tag.
Voice mail
Voice mail is an efficient way to communicate. Again, five tips:
- Always be prepared to leave a message. Jot down your key message points before you call, to avoid stuttering and stammering.
- Be concise and to the point.
- State your name and the date, time, and purpose of your call.
- Enunciate clearly and speak slowly.
- State your name and phone number twice at the end of the message so the recipient doesn’t need to replay your message.
In many business settings, e-mail has almost replaced letters and memos. In many cases, an e-mail is a recipient’s first impression of you, so follow these tips:
- Make the subject line specific. This helps the reader prioritize the message and file it for easy retrieval.
- Use a greeting and a close. It’s more polite and less impersonal.
- Keep your message concise.
- Keep your tone polite and businesslike.
- Use your e-mail signature function, which provides several ways to contact you.
Text messages
This form of communication can be the most challenging and unpredictable. Some people send text messages routinely, while others may be unfamiliar with this method. You can’t go too far wrong if you take this advice:
- Get to the point quickly. No one wants to read a long message on a mobile phone.
- Don’t text during meetings. It’s rude to do so, and others can hear you clicking away or see the light from your screen.
- Consider the recipient before using text abbreviations. Some people may not understand text lingo.
- Consider the time when sending a text. Although you may be awake at 5 a.m., the sound of your incoming message might disturb a sleeping recipient.
- Don’t expect an immediate response to your text. If the message is time sensitive, pick up the phone instead.
Improving the way we speak with managers and physicians can go a long way toward career advancement and professional satisfaction. Common courtesy is just as essential in e-mail, voice mail, and text messages as in face-to-face communication. When you follow the guidelines I’ve given, you’ll elevate your professional communications a few notches.
Selected references
Canfield J, Switzer J. The Success Principles: How to Get from Where You Are to Where You Want to Be. New York, NY: Morrow; 2006.
Kramer M, Schmalenberg, C. Confirmation of a healthy work environment. Crit Care Nurse. 2008 Apr;28(2):56-63.
Pagana K. The Nurse’s Communication Advantage: How Business Savvy Communication Can Advance Your Nursing Career. Indianapolis, IN: Sigma Theta Tau International; 2011.
Pagana K. The Nurse’s Etiquette Advantage: How Professional Etiquette Can Advance Your Nursing Career. Indianapolis, IN: Sigma Theta Tau International; 2008.
A keynote speaker, Kathleen D. Pagana is a professor emeritus at Lycoming College in Williamsport, Pennsylvania, and president of Pagana Keynotes and Presentations. She is the author of The Nurse’s Communication Advantage and The Nurse’s Etiquette Advantage. To contact her, visit www.KathleenPagana.com.
Read More