By Rosalyn Jordan, RN, BSN, MSc, CWOCN, WCC, and Marci Christian, BBE
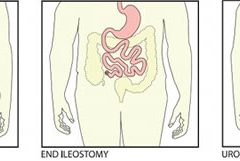
Any patient with a fecal or urinary ostomy may experience complications on the skin surface around the stoma. These complications may occur lifelong, although they’re more common during the first 5 years after the initial ostomy surgery. Causative factors include infection, trauma, certain diseases, and chemical irritation; most of these problems stem from the pouching system or pouch leakage.
Peristomal skin complications can cause a wide range of signs and symptoms, from skin discoloration to polyp-like growths, from erythema to full-thickness wounds. They can lead to discomfort, pain, poor self-image, social isolation, and impaired quality of life, not to mention additional care costs.
Incidence and types of these complications are hard to compare or contrast across multiple patients. Until recently, no standardized assessment or documentation tools were available to characterize or define complications. For this reason, reported rates ranged widely, from 10% to 70%. And because no designated common language or categories related to peristomal skin complications existed, documentation was inconsistent.
Download “How to Use” education program for the Ostomy Skin Tool
Ostomy Skin Tool
In the late 2000s, a group of nurses experienced in caring for ostomy patients worked with the World Council of Enterostomal Therapists to develop a resource called the Ostomy Skin Tool, which clinicians can use to categorize and describe peristomal skin complications in a consistent, objective manner. The tool also provides a common language for documentation.
The Ostomy Skin Tool has three major assessment domains—discoloration (D), erosion/ulceration (E), and tissue overgrowth (T), known collectively as DET. The DET combined rating ranges from normal, rated 0, to the worst condition possible, rated 15. Mild DET complications are documented as less than 4, moderate as less than 7, and severe as 8 or higher. (See Using the Ostomy Skin Tool by clicking the PDF icon above.)
The tool describes four categories of peristomal complications:
• chemical irritation
• mechanical trauma
• disease-related complications
• infection-related complications.
Chemical irritation
Chemical irritation can stem from irritants (as in contact dermatitis) or allergic reactions (allergic dermatitis). The most likely cause of chemical dermatitis is effluent leakage (feces or urine) from the colostomy, ileostomy, or urostomy, in which effluent comes in contact with peristomal skin. Other potential causes include contact with soap, certain adhesives, and adhesive removers.
The major treatment of chemical irritation is identification and removal of the offending agent, followed by patient and caregiver education on the new pouching procedure the patient must use. Follow-up assessment also is recommended. In a 2010 study that followed 89 patients for 1 year after ostomy surgery, about 50% of subjects experienced peristomal skin complications, most of them from pouch leakage. Another investigator estimated that 85% of ostomy patients experience pouch leakage at some time during their lives. Pouch leakage usually occurs when stool is extremely liquid (for instance, ileostomy effluent). Other causes of pouch leakage include wearing a pouch more than half full of effluent and abdominal contours that aren’t level. Besides changes in the pouching system, treatment may entail adding products to the pouching system or removing certain agents.
Some patients experience allergic dermatitis in reaction to products used in the pouching system (such as skin barriers, belts, pouch closures, or adhesives). However, allergic dermatitis is rare. One 2010 study suggested allergic reactions to these products occur in only about 0.6% of patients with peristomal skin irritation. Most major ostomy product manufacturers provide a patch test on request to help identify allergic conditions. Once the offending product is discontinued, allergic dermatitis should resolve rapidly.
Mechanical trauma
Mechanical trauma usually results from either the pouching system itself or its removal. It also may result from harsh or multiple skin-barrier removals, pressure from convex rings or pouches, and abrasive cleansing techniques. Some researchers believe the stronger the adhesive barrier and the more often a pouch is changed, the greater the risk of epidermal damage.
Mechanical trauma may present as a partial-thickness ulcer caused by pressure, shear, friction, tearing, or skin stripping. Patients with fragile skin are susceptible to mechanical trauma, so less aggressive pouching systems may be preferred for them. Of course, if the pouching system is changed, the patient or caregiver needs to learn about the new system.
Disease-related complications
Disease-related peristomal complications may be linked to preexisting skin conditions, such as psoriasis, eczema (atopic dermatitis), or seborrheic dermatitis. Hyperplasia also may occur. This overgrowth of cells, which may appear as gray or reddish brown pseudoverrucous lesions, usually is linked to urinary ostomies, although it can occur with fecal ostomies as well. Vinegar soaks are the recommended treatment, in addition to a change in the pouching system and corresponding patient education.
Occasionally, other disease-related complications occur, including primary adenocarcinoma of the peristomal skin and peristomal pyoderma gangrenosum, a painful and problematic condition that presents as peristomal ulcers. Ulcer borders are well-defined with a bluish purple coloration at the edges. Infection must be ruled out, as this condition usually is linked to an autoimmune condition. Treatment includes pain management and, in most cases, a topical corticosteroid. Crohn’s disease also may manifest as a peristomal skin ulcer.
Infection-related complications
Infection-related complications may be bacterial or fungal. Two common peristomal skin infections are folliculitis and Candida fungal infections. An infection of the hair follicle that causes pustules, folliculitis usually stems from traumatic hair pulling in the peristomal area during pouch removal. It may warrant a prescribed antibiotic, along with patient teaching regarding proper hair removal using an electric razor.
Candida infections may arise because peristomal skin provides a warm, dark, moist environment that promotes fungal growth. These infections appear as erythema with pustules or papules and satellite lesions. Treatment usually involves antifungal powder and use of the crusting technique to secure the pouching system. (See Using the crusting technique by clicking the PDF icon above.)
Management
Many complications are well advanced by the time patients seek assistance, perhaps because they don’t understand the significance of their symptoms and think they can manage the problem themselves. In some cases, they don’t know where to turn for assistance. Commonly, the complication progresses to the point where the patient goes to the emergency department or (particularly during the immediate postoperative period) needs to be readmitted for treatment. The best way to manage peristomal skin complications is to prevent them in the first place. (See Preventing peristomal skin complications by clicking the PDF icon above.)
Patient education
Over the past 20 years, hospital stays for ostomy surgery patients have decreased from about 2 weeks to less than 5 days. Reduced stays decrease the time available for caregivers to teach patients and family members how to empty and change the pouch. They need alternative education covering (among other topics) how to recognize peristomal skin complications and when to seek help. Not only do these complications require vigilant self-observation, but many patients don’t understand their implications or how rapidly they can worsen. In some cases, the first symptoms are itching and redness under the skin barrier. Fortunately, some patients may know or remember that itching, burning, stinging, reddened, or weeping peristomal skin requires professional attention. They can avoid serious complications by seeking assistance early, such as right after noticing pouch leakage.
Early treatment can reduce the cost of treatment. In a 2012 study, researchers estimated care costs related to peristomal skin complications for a 7-week treatment period, using the Ostomy Skin Tool as a reference. Severe complications (those with a DET score above 8) cost six times more to treat than mild cases (those with a DET score below 4) and 4.5 times more than moderate cases.
Along with early intervention by a trained ostomy care specialist, self-assessment by ostomy patients promotes a better quality of life, reduces pain, and may decrease care costs. Clinicians’ use of the Ostomy Skin Tool to assess and document peristomal skin complications promotes more reliable, objective, comparable assessment data for reporting.
Selected references
Al-Niaimi F, Lyon CC. Primary adenocarcinoma in peristomal skin: a case study. Ostomy Wound Manage. 2010;56(1):45-7.
Burch J. Management of stoma complications. Nurs Times. 2011;107(45):17-8, 20.
Jemec GB, Martins L, Claessens I, et al. Assessing peristomal skin changes in ostomy patients: validation of the Ostomy Skin Tool. Br J Dermatol. 2011; 164;330-5.
Jones T, Springfield T, Brudwick M, Ladd A. Fecal ostomies: practical management for the home health clinician. Home Healthc Nurse. 2011;29(5):306-17.
Martins L, Samai O, Fernandez A, et al. Maintaining healthy skin around an ostomy: peristomal skin disorders and self-assessment. Gastrointest Nurs. 2011;
9(2):9-13.
Martins L, Tavernelli K, Serrano JLC. Introducing a peristomal skin assessment tool: The Ostomy Skin Tool. World Council Enterostomal Therapists J. 2008;28(2):3-13.
Meisner S, Lehur P, Moran B, et al. Peristomal skin complications are common, expensive, and difficult to manage: a population based cost modeling study. PLoS One. 2012;7(5):e37813.
Nybaek H, Jemec GB. Skin problems in stoma patients. J Eur Acad Dermatol Venereol. 2010;24(3):249-57.
Omura Y, Yamabe M, Anazawa S. Peristomal skin disorders in patients with intestinal and urinary ostomies: influence of adhesive forces of various hydrocolloid wafer skin barriers. J Wound Ostomy Continence Nurs. 2010;37(3):289-98.
Ratliff CR. Early peristomal skin complications reported by WOC nurses. J Wound Ostomy Continence Nurs. 2010;37(5):505-10.
Shabbir J, Britton DC. Stomal complications: a literature overview. Colorectal Dis. 2010;12(10):958- 64.
Wound, Ostomy, Continence Clinical Practice Ostomy Subcommittee. Peristomal skin complications: Best practice for clinicians. Mt. Laurel, NJ; 2007.
The authors work for RecoverCare, LLC, in Louisville, Kentucky. Rosalyn Jordan is director of clinical education and Marci Christian is a clinical associate product specialist.
Read More