By Steve Norton, CDT, CLT-LANA
Editor’s note: Part 1 of this series, published in the September-October issue, discussed lymphedema pathology and diagnosis. This article, Part 2, covers treatment.
Traditional treatment approaches
Traditionally, lymphedema treatment has been approached without a clear understanding of the underlying structure and function of lymphatic tissues. Ineffective traditional treatments include elevation, elastic garments, pneumatic pumps, surgery, diuretics, and benzopyrones (such as warfarin). Because many traditional treatments are still overused and some may be appropriate for limited use, it’s important for clinicians to understand these approaches.
Elevation
As a sole therapy for lymphedema, elevation of the affected part provides only short-lived results. Ever-increasing macromolecular wastes retain water against the effects of gravity. Increased interstitial colloid osmotic pressure must be addressed by interventions targeted at improving lymphatic function—not just a position change. Otherwise, lymphedema will progress. Furthermore, elevation alone is impractical, promotes deconditioning, and alters lifestyle for prolonged periods.
Elastic garments
Elastic garments prove inadequate because they attempt to treat lymphedema with compression alone. Medically correct garments are engineered with thoughtful attention to high-quality textiles and offer gradient support, which promotes proximal flow. However, without precise tissue stimulation leading to improved lymphangioactivity (lymph-vessel pulsation), macromolecular wastes can’t be removed.
Interstitial pressure increases caused by compression garments impede further fluid accumulation. When these garments are removed, the spontaneous girth increase causes an imprecise fit, and the garment rapidly leads to a countertherapeutic effect. Furthermore, compression garments don’t combat the osmotic forces generated by ever-increasing interstitial wastes. Except in patients diagnosed with stage 0 or stage 1 lymphedema, disease progression involving metaplasia ensues. Although elastic compression garments are a cornerstone of long-term management, they shouldn’t be used as a stand-alone treatment.
Pneumatic compression pump
Formerly, the pneumatic compression pump (PCP) was considered the standard of care for lymphedema. However, when inflated, the pump doesn’t increase the frequency of lymph-vessel contraction or enhance lymph capillary absorption. What’s more, accelerated fibrosis development and rapid tissue refilling occur when a PCP is removed. Also, PCP use disregards the ipsilateral territory of the excised regional nodes, effectively dumping fluid from the leg into the trunk. A PCP is appropriate only when nothing else is available, as it may worsen the patient’s condition.
Surgery
Surgical approaches to treating lymphedema involve either excisional (debulking) or microsurgical techniques. The most extensive surgical technique, the radical Charles procedure, completely debulks all involved tissue down to the muscle fascia. Split-thickness grafts are then harvested from excised skin and donor sites, and applied to the fascia to achieve so-called limb reduction.
Most debulking procedures have been applied to lower-extremity lymphedema and offer poor cosmetic results. Less radical surgeries favor long incisions, preserving the skin but excising subcutaneous edematous portions to reduce girth. Although less cosmetically alarming, these procedures effectively amputate the subcutaneous space where lymph vessels reside. Other surgical approaches are beyond the scope of this article.
Generally, surgery isn’t a good approach for any patient, as it’s linked to significant morbidity, such as skin necrosis, infection, and sensory changes. In the future, less invasive procedures may be available that yield significant improvement without these adverse effects.
Diuretics
Although diuretics are prescribed appropriately to address water-rich edemas of venous origin, they disregard the fact that lymphedema is a protein-rich edema. Long-term, high-dose diuretic therapy leads to treatment-resistant limbs, similar to those that have received intensive pneumatic compression.
Benzopyrones
Benzopyrones such as warfarin decrease swelling by combating protein accumulation in fluid. Such drugs have undergone clinical trials abroad. Their mechanism is to promote macrophage migration into interstitial fluid, as well as subsequent proteolysis. Due to significant risk of liver damage or failure, benzopyrones haven’t been approved for treating lymphedema.
Complete decongestive therapy: The current treatment approach
Currently, the gold standard for lymphedema treatment is complete decongestive therapy (CDT). Michael Foeldi and Etelka Foeldi, who originated this method, discovered a unique symbiotic relationship among five distinct modalities that addresses the challenges of lymphedema treatment. In 1989, CDT was brought to the United States by Robert Lerner and has become the mainstay of lymphedema treatment here.
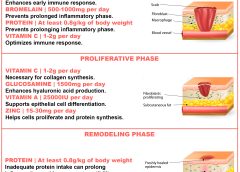
CDT is a two-phase approach involving an intensive clinical effort followed by a semi-intensive home-care program geared toward autonomous management, stabilization, and continual improvement. It involves manual lymph drainage (MLD), compression bandaging, exercise, skin and nail hygiene, and self-care education. (See Phases of complete decongestive therapy by clicking the PDF icon above.)
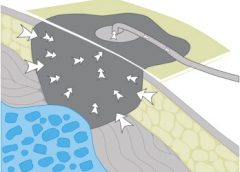
Manual lymph drainage
A type of soft-tissue mobilization, MLD provides skin traction, stimulating superficial lymph vessels and nodes. Lymph capillaries contain large inter-endothelial inlets called swinging tips, akin to overlapping shingles. Each overlapping cell is tethered to the interstitial matrix by anchoring filaments, so that fluid increases cause immediate distention and lymph inflow. Manual skin traction using MLD promotes greater lymph fluid uptake by stretching these filamentous structures, opening the swinging tips.
MLD also provides extrinsic stimulation of the lymphangion (the segment of a lymph vessel between a distal and proximal valve), drawing fluid into the system at the capillary level and promoting flow at the vessel level toward regional lymph nodes. Usually, these segments contract and relax in a rhythmic fashion six times per minute. MLD triples this output to 18 or 20 times per minute, greatly enhancing systemic transport.
MLD requires intensive daily treatment sessions to strengthen collateral flow as a pathway to circumventing surgical or developmental lymphatic disruption. Treatment strategies further recruit more deeply situated lymphatics such as the thoracic duct, as well as lumbar trunks that empty at the juncture of the internal jugular and subclavian veins to improve global uptake. MLD thus stimulates deeper vessel angioactivity to help drain the superficial vessels that drain toward them.
Compression bandaging
Compression bandaging provides tissue support after MLD to prevent reflux, slow new fluid formation, and mechanically soften fibrotic areas. Bandaging techniques provide a high working pressure to harness the muscle and joint pumps as a propellant for lymph while resisting retrograde flow created by gravity and centrifugal forces during movement. Pure cotton materials coupled with specialized padding create a soft, castlike environment, which confines swollen tissues without constriction. By relying on high working pressure and low resting pressures to decrease limb swelling, this strategy achieves greater control over intensity (level of compression/pressure exerted), with little to no soft-tissue injury or discomfort.
The patient wears this bulky inelastic complex after each MLD treatment until the next day’s session to ensure limb-volume reduction in a stable, linear fashion. Once a plateau is reached, tissue stabilization and self-care education are the goals of additional sessions.
Exercise
Exercise always must be done with adequate support to counteract fluid formation. During the intensive CDT phase, limbs are bandaged to provide complete around-the-clock containment. Gentle exercises encourage blood flow into the muscle; during muscle contraction, this creates a favorable internal pressure that effectively squeezes the subcutaneous space between the bandage wall and muscle. Because every bandage strives to provide a gradient of support, fluid tends to drain proximally to the bandage—in most cases, to the trunk.
Skin and nail hygiene
Without intact, well-hydrated skin, cellulitic infections occur in many lymphedema patients whose immune response has been diminished by regional lymphadenectomy or inherited deficiencies. To prevent infection caused by avoidable external events, patients receive clear guidelines to reinforce appropriate behavior. As most cellulitis results from resident skin pathogens (streptococci and staphylococci), maintaining a low skin pH helps control colonization. Ways to avoid recurrent infections include maintaining an acid mantle on the skin using low-pH-formulated lotions and avoiding injury from daily tasks that may scratch, puncture, burn, or abrade the skin. Patients should receive lists of self-care precautions at the time of treatment.
Self-care education
Because lymphedema is a chronic condition, patients must receive self-care education for daily management to avoid lymphedema destabilization, which can lead to tissue saturation and subsequent skin changes. Therapists must provide patients with appropriate self-care tools and knowledge to maintain adequate treatment results. Teaching topics include how to apply and remove compression garments and bandages and how to exercise safely, preserve skin integrity, monitor for infection, and respond appropriately to infection and significant changes in limb mobility.
An underrecognized and mistreated problem
Lymphedema remains an underrecognized and mistreated condition, even though CDT yields safe, reliable results. Early detection, accurate staging, proper diagnosis, and appropriate treatment can slow the inevitable progression of lymphedema. Wound care specialists should adapt wound therapy to address not just the wound but the edematous environment responsible for delayed wound resolution.
Selected references
Al-Niaimi F, Cox N. Cellulitis and lymphedema: a vicious cycle. J Lymphoedema. 2009;4:38-42.
Browse N, Burnand KG, Mortimer PS. Diseases of the Lymphatics. London: Hodder Arnold; 2003.
Casley-Smith JR, Casley-Smith JR. Modern Treatment for Lymphoedema. 5th ed. The Lymphoedema Association of Australia; 1997.
Cooper R, White R. Cutaneous infections in lymphoedema. J Lymphoedema. 2009:4:44-8.
Foeldi M. Foeldi’s Textbook of Lymphology: For Physicians and Lymphedema Therapists. 3rd ed. St. Louis, MO: Mosby; 2012.
International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema. Consensus Document of the International Society of Lymphology. Lymphology. 2009 Jun;42(2):51-60.
Leduc A, Bastin R, Bourgeois P. Lymphatic reabsorption of proteins and pressotherapies. Progress in Lymphology XI. 1988:591-2.
National Lymphedema Network Medical Advisory Committee. Position Statement: Lymphedema Risk Reduction Practices. Revised May 2012. http://www.lymphnet.org/pdfDocs/nlnriskreduction.pdf. Accessed September 5, 2012.
Pappas CJ, O’Donnell TF Jr. Long-term results of compression treatment for lymphedema. J Vasc Surg. 1992 Oct;16(4):555-62.
Whittlinger H. Textbook of Dr. Vodder’s Manual Lymphatic Drainage. Vol 1. 7th ed. New York, NY: Thieme; 2003.
Steve Norton is cofounder of Lymphedema & Wound Care Education and executive director of the Norton School of Lymphatic Therapy in Matawan, New Jersey.
Read More