Optimizing nutritional status is a key strategy both in preventing and managing pressure ulcers. In patients across all care settings, compromised nutrition— as from poor intake, undesired weight loss, and malnutrition—increases the risk of pressure ulcers. It contributes to altered immune function, impaired collagen synthesis, and decreased tensile strength. In many cases, malnutrition also contributes to wound chronicity and increases the risk for delayed and impaired wound healing. In patients with chronic wounds, such as pressure ulcers, a chronic inflammatory state can induce catabolic metabolism, malnutrition, and dehydration. (more…)
Read MoreTag: pressure injury
Clinical Notes: ostomy, pressure ulcer, burn treatment
Self-management ostomy program improves HRQOL
A five-session ostomy self-care program with a curriculum based on the Chronic Care Model can improve health-related quality of life (HRQOL), according to a study in Psycho-Oncology.
“A chronic care ostomy self-management program for cancer survivors” describes results from a longitudinal pilot study of 38 people. Participants reported sustained improvements in patient activation, self-efficacy, total HRQOL, and physical and social well-being. Most patients had a history of rectal cancer (60.5%) or bladder cancer (28.9%). (more…)
Read MoreBuzz Report: Latest trends, part 2
Keeping clinicians up-to-date on clinical knowledge is one of the main goals of the Wild on Wounds (WOW) conference held each September in Las Vegas. Every year, I present the opening session, called “The Buzz Report,” which focuses on the latest-breaking wound care news—what’s new, what’s now, and what’s coming up. I discuss new products, practice guidelines, resources, and tools from the last 12 months in skin, wound, and ostomy management.
In the January issue, I discussed some of the updates from my 2015 Buzz Report. Now I’d like to share a few more, along with some of my favorite resources. (more…)
Read MoreEmpowering patients to play an active role in pressure ulcer prevention
Developing a pressure ulcer can cause the patient pain, lead to social isolation, result in reduced mobility, and can even be fatal. According to the Agency for Healthcare Research and Quality, estimated costs for each pressure ulcer range from $37,800 to $70,000, and the total annual cost of pressure ulcers in the United States is an estimated $11 billion.
Nurses understand their role in preventing pressure ulcers, but what role do patients play in the prevention plan? Nurses need to empower the patient to be an active member in health promotion activities and participate in prevention measures. In this article, I highlight the importance of incorporating pressure ulcer prevention into patient education for high-risk patients as a way to empower patients. Empowered patients can help improve outcomes and reduce overall costs of this hospital-acquired complication. (more…)
Read MoreRestorative nursing programs help prevent pressure ulcers
Immobility affects all our body systems, including our skin. According to the National Pressure Ulcer Advisory Panel, many contributing factors are associated with the formation of a pressure ulcer, with impaired mobility leading the list.
So what can clinicians do to prevent harm caused by immobility? One often-overlooked strategy is a restorative nursing program. (See About restorative nursing.)
Moving up the time line
Most patients who score poorly for mobility and/or activity impairments on the Braden Scale for Predicting Pressure Ulcer Risk are referred to physical therapy, but too often a restorative nursing program (more…)
Read MoreProve the Value Program
Clinician Resources: falls, npuap, patient safety, civility
End your year by checking out these resources for your practice.
Sentinel event alert for falls
As part of its sentinel event alert “Preventing falls and fall-related injuries in health care facilities,” The Joint Commission has assembled information and multiple resources, including:
- analysis of contributing factors for falls
- evidence-based suggestions for improvement
- Joint Commission requirements relevant to falls
- links to toolkits and protocols
- an infographic on preventing falls.
Clinical Notes
Mild compression diabetic socks safe and effective for lower extremity edema
Diabetic socks with mild compression can reduce lower extremity edema in patients with diabetes without adversely affecting arterial circulation, according to a randomized control trial presented at the American Diabetes Association 75th Scientific Sessions Conference. (more…)
Read MoreClinician Resources: NPUAP, Pressure Ulcer Treatment, NIOSH
The resources below will help you address issues in your practice.
NPUAP position statement on hand check for bottoming out
Use of the hand check to determine “bottoming out” of support systems should be limited to static air overlay mattresses, according to a position statement from the National Pressure Ulcer Advisory Panel (NPUAP). (more…)
Read MoreClinician Resources: Nutrition, Treatment Algorithms, Pressure Ulcer Prevention
Check out these resources for your practice.
Be a nutrition champion
One in three patients enters a hospital malnourished. Fight malnutrition by viewing six short videos from the Alliance to Advance Patient Nutrition, including “Rapidly Implement Nutrition Interventions” and “Recognize and Diagnose All Patients at Risk of Malnutrition.” The videos show how to collaborate with the care team to become champions of nutrition and help improve patient outcomes. Watch the videos online or download them for later viewing. (more…)
Read MoreImmobility as the root cause of pressure ulcers
By Jeri Lundgren, BSN, RN, PHN, CWS, CWCN
Many factors can contribute to the formation of a pressure ulcer, but it’s rare that one develops in an active, mobile patient. As the National Pressure Ulcer Advisory Panel 2014 guidelines state, “Pressure ulcers cannot form without loading, or pressure on the tissue. Extended periods of lying or sitting on a particular body part and failure to redistribute the pressure can lead to ischemia and therefore tissue damage.” Thus, immobility is frequently the root cause of pressure ulcer development. (more…)
Read MorePreventing pressure ulcers in pediatric patients
By Roxana Reyna, BSN, RNC-NIC, WCC, CWOCN
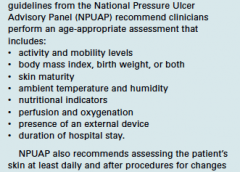
As wound care clinicians, we are trained—and expected—to help heal wounds in patients of any age and to achieve positive outcomes. Basic wound-healing principles apply to all patients, whatever their age or size. The specific anatomy and physiology of vulnerable pediatric patients, however, requires detailed wound care. Unfortunately, little evidence-based research exists to support and direct the care of pediatric patients with pressure ulcers. This article describes efforts to reduce pressure ulcers in pediatric patients at Driscoll Children’s Hospital (DCH) in Corpus Christi, Texas. (more…)
Read More