On April 13, 2016, the National Pressure Ulcer Advisory Panel (NPUAP) announced changes in pressure ulcer terminology and staging definitions. Providers can adapt NPUAP’s changes for their clinical practice and documentation, but it’s important to note that, as of press time, the Centers for Medicare & Medicaid Services (CMS) has not adopted the changes. This means that providers can’t use NPUAP’s updates when completing CMS assessment forms, such as the Minimum Data Set (MDS) or Outcome and Assessment Information Set (OASIS). Instead, they must code the CMS assessment forms according to current CMS instructions and definitions. In addition, there is no ICD-10 code for pressure injury. (more…)
Read MoreSearch Results for: documentation
2016 Journal: March – April Vol. 5 No. 2
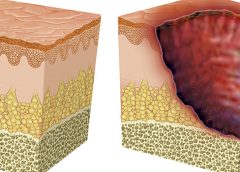
A pressure ulcer by any other name
Just when we think we’ve figured out pressure ulcer staging, it changes again. In April 2016, the National Pressure Ulcer Advisory Panel (NPUAP) held a consensus conference on staging definitions and terminology. The purpose: to analyze and discuss the rationale for the panel’s changes. One of the key changes is replacing the term “pressure ulcer” with “pressure injury.” So instead of calling it a pressure ulcer staging system, NPUAP will refer to it as a pressure injury staging system. The panel explained that the new terminology “more accurately describes pressure injuries to both intact and ulcerated skin.” Other changes include: (more…)
Read MoreNutritional considerations in patients with pressure ulcers
Optimizing nutritional status is a key strategy both in preventing and managing pressure ulcers. In patients across all care settings, compromised nutrition— as from poor intake, undesired weight loss, and malnutrition—increases the risk of pressure ulcers. It contributes to altered immune function, impaired collagen synthesis, and decreased tensile strength. In many cases, malnutrition also contributes to wound chronicity and increases the risk for delayed and impaired wound healing. In patients with chronic wounds, such as pressure ulcers, a chronic inflammatory state can induce catabolic metabolism, malnutrition, and dehydration. (more…)
Read MoreBuzz Report: Latest trends, part 2
Keeping clinicians up-to-date on clinical knowledge is one of the main goals of the Wild on Wounds (WOW) conference held each September in Las Vegas. Every year, I present the opening session, called “The Buzz Report,” which focuses on the latest-breaking wound care news—what’s new, what’s now, and what’s coming up. I discuss new products, practice guidelines, resources, and tools from the last 12 months in skin, wound, and ostomy management.
In the January issue, I discussed some of the updates from my 2015 Buzz Report. Now I’d like to share a few more, along with some of my favorite resources. (more…)
Read MoreEmpowering patients to play an active role in pressure ulcer prevention
Developing a pressure ulcer can cause the patient pain, lead to social isolation, result in reduced mobility, and can even be fatal. According to the Agency for Healthcare Research and Quality, estimated costs for each pressure ulcer range from $37,800 to $70,000, and the total annual cost of pressure ulcers in the United States is an estimated $11 billion.
Nurses understand their role in preventing pressure ulcers, but what role do patients play in the prevention plan? Nurses need to empower the patient to be an active member in health promotion activities and participate in prevention measures. In this article, I highlight the importance of incorporating pressure ulcer prevention into patient education for high-risk patients as a way to empower patients. Empowered patients can help improve outcomes and reduce overall costs of this hospital-acquired complication. (more…)
Read MoreTop 10 outpatient reimbursement questions
At the 2015 Wild on Wounds conference, the interactive workshop “Are You Ready for an Outpatient Reimbursement Challenge?” featured a lively discussion among participants about 25 real-life reimbursement scenarios. Here are the top 10 questions the attendees asked, with the answers I provided.
Q Why is it necessary for qualified healthcare professionals (QHPs) such as physicians, podiatrists, nurse practitioners, physician assistants, and clinical nurse specialists to identify the place of service where they provide wound care services and to correctly state the place of service on their claim forms? (more…)
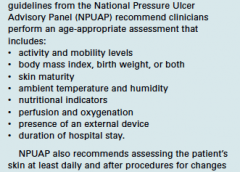
Read MorePreventing pressure ulcers in pediatric patients
By Roxana Reyna, BSN, RNC-NIC, WCC, CWOCN
As wound care clinicians, we are trained—and expected—to help heal wounds in patients of any age and to achieve positive outcomes. Basic wound-healing principles apply to all patients, whatever their age or size. The specific anatomy and physiology of vulnerable pediatric patients, however, requires detailed wound care. Unfortunately, little evidence-based research exists to support and direct the care of pediatric patients with pressure ulcers. This article describes efforts to reduce pressure ulcers in pediatric patients at Driscoll Children’s Hospital (DCH) in Corpus Christi, Texas. (more…)
Read MoreGet the ‘SKINNI’ on reducing pressure ulcers
By Cindy Barefield, BSN, RN-BC, CWOCN
Like many hospitals, Houston Methodist San Jacinto Hospital uses national benchmarks such as the National Database of Nursing Quality Indicators (NDNQI®) to measure quality outcomes. Based on benchmark reports that showed an increased trend of pressure ulcers in critically ill patients in our hospital, the clinical nurses in our Critical Care Shared Governance Unit-Based Council (CCSGUBC) identified an improvement opportunity. (more…)
Read MoreFinding common ground: Surviving wound care communication
By Jennifer Oakley, BS, RN, WCC, DWC, OMS
The author describes how to overcome challenges to effective communication in the healthcare setting.
Accurate communication among healthcare professionals can spell the difference between patient safety and patient harm. Communication can be a challenge, especially when done electronically. With an e-mail or a text, you can’t hear the other person’s voice or see the body language, so it’s easy to misinterpret the words. (more…)
Read MoreClinician Resources: March-April 2015
Below are resources you may find helpful to your practice.
AHRQ’s Safety Program for Nursing Homes: On-Time Prevention
The Agency for Healthcare Research and Quality (AHRQ) has established “AHRQ’s Safety Program for Nursing Homes: On-Time Prevention,” designed to improve long-term care by turning daily documentation into useful information that enhances clinical care planning.
On-Time uses electronic medical records to develop weekly reports that identify residents at risk for common adverse events in nursing homes to help clinical staff intervene early. Facilitators help the team integrate these reports into clinical decision making to improve care planning.
For each adverse event, the website provides a description of the reports and suggested meetings and huddles where the reports may be used, the functional specifications for programming the reports, description of implementation tools, and a 2-day training curriculum for facilitators.
Sleep times guidelines
The National Sleep Foundation has issued new recommendations for appropriate sleep durations. Check below to see if your patients—and you—are getting enough sleep:
• newborns (0-3 months): 14-17 hours
• infants (4-11 months): 12-15 hours
• toddlers (1-2 years): 11-14 hours
• preschoolers (3-5 years): 10-13 hours
• school-age children (6-13 years): 9-11 hours
• teenagers (14-17 years): 8-10 hours
• younger adults (18-25 years): 7-9 hours
• adults (26-64 years): 7-9 hours
• older adults (65+ years): 7-8 hours.
Access “National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary” in Sleep Health.
Venous ulcer resources
The website for the Association for the Advancement of Wound Care (AAWC) has several resources related to venous ulcers:
• AAWC Venous Ulcer Guideline 3.12
• AAWC Venous Ulcer Guideline Evidence 6.13
• AAWC Venous Ulcer Guideline Algorithm Presentation 8.13
• AAWC Venous Ulcer Guideline Checklist 7.13.
The resources are available at no cost.
Wound care app
The Johnson & Johnson Wound Care Resource™ App helps patients identify, track, and provide recommendations on wound care treatment.
The free app includes treatment videos and coupons to help patients save on wound care treatment supplies. The app is available for download on iTunes.
What does it mean to participate in a wound care clinical trial?
By Susan Beard, RN, BS, CWOCN
Suppose you’re reading an article on a new product that states the product has been through a series of clinical trials before marketing. What does this mean? Who was involved? As a clinician, could you initiate or be involved in a clinical trial of a new product? Who are clinical trial subjects, and what’s it like for them to be involved in a clinical study?
A clinical trial starts as an idea. As clinicians, we often use our critical-thinking skills to imagine a product or method of practice we think could be created or improved on to better meet our patients’ needs. The idea begins to grow and a series of events begins. (more…)
Read More