By Nancy J. Brent, MS, RN, JD
Often nurses get named in a lawsuit when they are involved in clearly negligent conduct that causes an injury to or the death of a patient. Examples include administering the wrong medication to the wrong patient or not positioning a patient correctly in the operative suite prior to surgery. Sometimes, however, the negligent behavior of a nurse is not as clear to the nurse involved in the care of the patient.
That was apparently the circumstance in the reported case, Olsten Health Services, Inc v. Cody.¹ In September 2000, Mr. Cody was the victim of a crime that resulted in paraplegia. He was admitted to a rehabilitation center and discharged on November 15, 2000. His physician ordered daily home health care services in order to monitor his “almost healed” Stage 2 pressure ulcer.² The home health care agency assigned a registered nurse (RN) to Mr. Cody and, after Mr. Cody’s healthcare insurance company would not approve daily visits, a reduced visit plan was approved by Mr. Cody’s physician.
A progressive problem
On November 16, 2000, the nurse visited Mr. Cody for the first time. During that visit, she did an admission assessment and noted that the pressure ulcer, located at the area
of the tailbone, measured 5 cm by 0.4 cm wide and 0.2 cm deep. She believed the pressure ulcer could be completely healed within 3 weeks. The nurse called Mr. Cody’s physician and left him a voice message concerning her visit and her findings.
On November 19, a second visit took place and the nurse observed and documented that Mr. Cody’s pressure ulcer was “100%” pink and no odor was detected.
On November 20, she attempted another visit but did not see Mr. Cody because the front gate surrounding his home was locked. The nurse buzzed the gate doorbell several times to no avail. She left a note on the front gate for the Cody family and left a voice message for Mr. Cody’s physician.
The next visit took place on November 21. The pressure ulcer was now only “90% pink” and had a “fetid” odor; this condition did not improve over the next 24 hours. The nurse documented this fact in her nurses’ notes. Again, she left a voice mail message for the physician concerning these findings.
The nurse could not get into the house on November 23, the next scheduled visit, so she again left a note on the house gate and left a voice mail message for the physician.
On November 24, the home health care nurse saw Mr. Cody and observed the pressure ulcer to be “90% pink” but the “fetid” odor was still present. In addition, Mr. Cody’s right lower extremity was swollen. She was concerned that the wound care that was to be done by the family or the health aide was not being done. Even so, she did not contact Mr. Cody’s physician or the patient again until November 27.
Mr. Cody’s pressure ulcer on November 27 had no odor but the home health aide who was also caring for Mr. Cody told the nurse that he was “very cold and having chills.” The nurse did not document this reported observation in her nurses’ notes.
Attempts to visit Mr. Cody on November 28 and 29 were again unsuccessful because of the locked gate at the front of the house. No one answered the buzzer, either. The nurse left another note on the house gate and left a voice mail message for the physician.
When the nurse saw Mr. Cody on November 30, she observed that the ulcer had “serious changes”: an increase in the serous drainage from the wound; the wound had a “fetid” odor; 80% of the wound was necrotic; the necrotic tissue was “undermined”; and the wound was significantly larger—9 cm by 8 cm wide and 1 cm deep.3 She left a voice mail message for Mr. Cody’s physician, but did not alter her visits to Mr. Cody’s home or attempt to see him over the next 2 days.
Admission to hospital
When the nurse did visit Mr. Cody on December 1, the pressure ulcer consisted of 40% necrotic tissue. She then told the family to take Mr. Cody to the physician’s office. Later that same day he was admitted to the hospital with a Stage 4 pressure ulcer that reached his tailbone. After 3 weeks of treatment, the ulcer measured 20 cm by 30 cm.
Mr. Cody endured many procedures during the following years to treat his
ulcer, but it never really healed. A “flap” enclosure was done to try to cover the wound.
Lawsuit
Mr. Cody sued the home health care company, alleging that the employees breached the standard of care by failing to appropriately diagnose and treat/or to prevent the formation or aggravation of pressure ulcers, resulting in severe and significant injury to him.
Verdict
The Florida Court of Appeals affirmed the trial court’s verdict in favor of Mr. Cody—a $3,050,000 verdict in economic damages4—on several legal bases, the most important for the purposes of this article being that the home health care agency and its employees were negligent in the care of Mr. Cody.
Key testimony
Key testimony in reaching this verdict came from the expert testimony of an RN and certified wound care expert. The nurse expert testified unequivocally that the home health care nurse breached the standard of nursing care. She said that not contacting the physician personally about Mr. Cody’s condition and the family being overwhelmed about his condition, but instead leaving voice mail messages on an answering machine, did not meet the standard of nursing care in this situation.
Additionally, the nurse expert testified that the nurse caring for Mr. Cody failed to recognize the symptoms of his deteriorating condition and did not intervene when necessary to avoid the infection he suffered from the deteriorating wound, and that her failure to do so resulted in the development of the Stage 4 ulcer that never healed.
Take-away points
So, what does this case tell you as a wound care professional caring for someone who has a pressure ulcer?
- Meet the standard of care. You must always meet the standard of care when caring for a patient. That means your care must be what other ordinary, reasonable, and prudent nurses caring for a patient with a decubitus ulcer would do in the same or similar circumstances in the same or similar community. Clearly, the nurse did not meet this standard in her care of Mr. Cody.
- Document accurately and completely. Remember that the nurse did not document Mr. Cody’s condition when the home health aide reported it to her. This omission may not only have compromised Mr. Cody’s care. If the communication during the trial became an “I told her”/”I don’t remember being told” debate when each party testified about the communication, it surely caused a rift between the aide and the nurse during the trial proceedings. Such a disagreement between defendant employees always helps a plaintiff’s case.
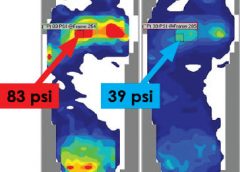
- Know that photographs can be used in court. This case used a specific form of evidence, demonstrative evidence: photographs taken of the pressure ulcer, which were admitted into evidence during the trial. The photographs were testified to by the wound care expert. In addition to her testimony, this evidence further showed the “natural and continual progression” of the ulcer as it existed on December 1, 2000.
- Understand the importance of expert testimony. In professional negligence cases, expert testimony is essential to establish the standard of care and to provide an opinion as to whether the standard of care was met or breached, the breach of which led to the injury to the patient. Typically, the attorney of a nurse cited in this type of case would want to use a certified wound care expert to support the care given. Apparently, the home care agency’s expert witness was not as convincing as the expert witness’s testimony for Mr. Cody.
Indeed, in this case, the expert witness’s testimony was invaluable and essentially secured a verdict for the plaintiff. Not only was the expert witness board certified but her testimony was credible, based on the evidence presented, and given after a careful review of Mr. Cody’s medical records, admission and discharge summaries from hospitals and health centers that provided care to Mr. Cody, the depositions of several doctors and nurses, and Mr. Cody’s deposition.
- Know your limits. The nurse’s conduct also stresses the importance of another legal principle—knowing the limits of your abilities and capabilities. Nowhere in the reported opinion are the RN’s qualifications listed or a reason given as to why she was selected to care for Mr. Cody. It is assumed she was not certified. Even basic nursing guidelines for wound care and communication to the physician were not followed. Why, then, did she agree to take this assignment? She did so not only at her own folly but to the detriment of Mr. Cody.
- Protect your patient. Last, and by no means least, this case stands for the principle that if you simply document something in the patient’s record that
is important regarding the patient’s well-being and you just leave voice mail messages for a physician about that “something,” such conduct is not adequate. By simply leaving messages and notes, this RN violated an age-old principle in the law of professional negligence.5
Your duty in any situation in which the patient is at risk for a foreseeable and unreasonable risk of harm is to prevent that harm from happening insofar as humanly possible. What those specific steps might be will depend on the circumstances and your patient’s condition. Remember, liability is always fact-specific. Although legal principles exist, how each applies to a particular situation may vary.
Mr. Cody was clearly at risk for a foreseeable and unreasonable risk of harm—the further deterioration of his pressure ulcer. The nurse would only have had to intervene sooner by, for example (and as testified to by the expert witness), personally talking with his physician, visiting the patient more frequently when the deterioration began, contacting social services to help the family with its “overwhelmed” feelings, and following up with the home health aide’s observations of Mr. Cody.
Think about this, too: Nowhere in the court of appeals’ record was it indicated that Mr. Cody’s family or the physician ever received the notes or voice mail messages left by the nurse.6 At a minimum, wouldn’t you as the nurse want to follow up and check if those communications had been received?
References
1. Olsten Health Services, Inc. v. Cody, 979 So. 2d 1221 (FL District Ct of Appeals) 2008. (pages 1-8). http://caselaw.findlaw.com/fl-district-court-of-appeal/1160380.html. Accessed June 22, 2012.
2. Id. at 1.
3. Id. at 4.
4. Id. at 2. The doctrine of comparative negligence was used in this case. This doctrine, adopted by most states, reduces a plaintiff’s recovery of money proportionally to the plaintiff’s degree of fault in causing the injury that is the basis of the suit (Blacks Law Dictionary, Second Pocket Edition, Bryan Garner, ed. St. Paul, MN: West; 2001). In this case, the home health care agency’s fault was attributed to be 70%. Mr. Cody’s degree of fault was assessed by the jury at 30%, most probably due to the inability of the home care nurse to be given access into the house on the days she visited and the family not providing the wound care required by Mr. Cody’s decubitus ulcer.
5. This age-old principle was established in a 1965 Illinois case, Darling v. Charleston Community Hospital, 211 N.E. 2d 353 (IL Supreme CT) 1965.
6. Tammelleo D. Treatment of decubitus ulcers botched: verdict for $3,050,000. Nurs Law Regan Rep. 2008;49(1):1.
Nancy J. Brent is an attorney in Wilmette, Illinois. The information in this article is for educational purposes only and does not constitute legal advice.
Read More