By Goranka Paula Bak, BSN, RN, ET, CWOCN
Every year, thousands of people of all ages have ostomy surgery in the United States. That means no matter where you work, you’re likely to care for patients with new ostomies and teach them to care for themselves. (See Why patients need ostomy surgery by clicking the PDF icon above.)
These patients present two challenges: staying up-to-date on ostomy equipment and procedures and having only 3 to 5 days after surgery to teach basic ostomy care to patients who are unlikely to be physically or emotionally ready to learn. This review and update of ostomy care should help you meet both challenges. Let’s start with the common types of stomas and ostomies.
Reviewing stoma types
The three common types of stomas are the end stoma, loop stoma, and double-barrel stoma. The patient’s surgeon decides on the most appropriate type based on the disease or injury, the amount of intestine available, and the patient’s health status.
To create an end stoma, the most common type, a surgeon creates a small opening in the abdominal wall, then resects the intestine and pulls it through the opening. Next, the surgeon turns the end of the intestine onto itself—somewhat like cuffing a sock—and sutures the stoma to the skin. Next to the stoma, the surgeon may create a mucous fistula, which secretes mucus from the nonfunctioning portion of the intestine.
A loop stoma is usually created for a temporary ostomy. The surgeon creates a small opening in the abdominal wall and pulls a loop of intestine through it. With an external rod or bridge placed under the loop to keep it from slipping back into the peritoneal cavity, the surgeon cuts the top of the loop to form the apex of the stoma. Next, the surgeon everts the intestine around the opening and sutures the stoma edges to the skin. After a few days, the rod is removed, and the stoma stays above skin level on its own.
Double-barrel stomas aren’t common in adults, but they are used frequently in neonates. For this type, a surgeon cuts through the bowel to create two separate end stomas, one to evacuate stool and the other to evacuate mucus. The two stomas can be placed next to each other, so one pouching system can be used for both. If the stomas are further apart, the patient may need two pouches. If mucus secretions are slight, you may be able to apply a nonadherent dressing after gently cleaning the stoma and peristomal skin, instead of using a pouch.
An ideal stoma protrudes above the skin surface and has a flat peristomal skin surface that allows the ostomy barrier to adhere to it. (See Characteristics of an ideal stoma by clicking the PDF icon above.) A healthy stoma is red and moist and looks like gum tissue. In fact, the entire alimentary canal from mouth to anus has the same type of tissue. Keep in mind that while cleaning a stoma, you’ll commonly see a small amount of bleeding, just as your gums may bleed when you brush your teeth too vigorously. If you note excessive bleeding, report it immediately.
Reviewing types of ostomies
The three most common types of ostomies you’ll see are a colostomy, an ileostomy, and a urostomy.
A surgeon creates a colostomy by making an opening in the large intestine and connecting it to the stoma. The location of the surgical opening will affect the consistency of the stool exiting the body through the stoma: The lower the opening, the firmer the consistency. A colostomy produces flatus because of the high bacterial content in the large intestine. A colostomy can be temporary or permanent, depending on the diagnosis and the patient’s ability to heal.
To create an ileostomy, a surgeon makes an opening in the small intestine and forms a stoma. Patients with ileostomies are prone to dehydration because a large amount of enzymatic fluid is discharged through the ileostomy instead of being absorbed in the disconnected large intestine. Teach your patient to be alert for the signs and symptoms
of dehydration—thirst; decreased urination; darker, concentrated urine; warm, flushed skin; fever; and malaise. Also, warn the patient to keep enzymatic effluent off the skin because it can quickly cause skin breakdown. As with a colostomy, an ileostomy may be temporary or permanent.
To create a urostomy, a surgeon removes the diseased bladder and uses a portion of resected small intestine to create a conduit. The ureters, which were connected to the bladder, are sutured into the resected small intestine so urine can exit the body through the stoma. Urostomies are permanent.
Choosing the right pouching system
An ostomy pouching system has two parts: an adhesive barrier that attaches to the skin around the stoma and a pouch connected to the barrier that collects effluent. Determining the right ostomy pouching system for your patients will depend on their needs and preferences. Let’s look at some of the important choices.
A pouching system may come in one or two pieces. With one-piece systems, the barrier (also called the wafer, flange, or baseplate) and pouch come as a single unit. (See One- and two-piece ostomy pouching systems by clicking the PDF icon above.) One-piece systems are easier to apply and more flexible. Plus, they’re flatter and thus more discreet.
With two-piece systems, the barrier and pouch are separate components that must be attached. Depending on the product, the patient may need to press the pouch onto the barrier or use a locking ring mechanism or an adhesive coupling system. Two-piece systems allow the patient to remove the pouch without removing the barrier. Also, a patient can apply a smaller pouch, such as a stoma cap or close-ended pouch, before exercise or intimate relations.
Today, ostomy pouching systems offer many options that weren’t available just a few years ago—options such as built-in, varying levels of convexity and integrated closures. Skin-friendly barriers now eliminate the need for accessory products, such as skin prep, ostomy powder, and stoma paste. By knowing the new options, you can help simplify the pouch application process for your patient and increase patient satisfaction.
Selecting barriers
Barriers may be cut-to-fit or precut. Cut-to-fit barriers are used during the postoperative period while the stoma size is changing and for oval or irregularly shaped stomas. Precut sizes are convenient for round stomas after they stabilize.
The choice of a barrier also depends on abdominal contours and the effluent consistency. A standard-wear barrier is appropriate for thicker output. An extended-wear barrier is better for loose or watery output and for problematic ostomies.
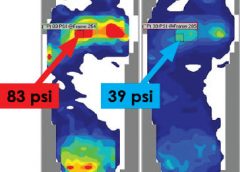
Convex barriers can be used to push down the peristomal skin and help the stoma project into the pouch. These barriers help ensure that the effluent goes into the pouch and not between the skin and the barrier, causing leakage.
For ostomies that are difficult to manage and frequently leak, you may select an ostomy belt. This device helps secure a convex pouching system by increasing its pressure. The plastic hooks at the end of the belt attach to the belt loops of the pouching system. Depending on the manufacturer, the belt loops may be on the barrier or the pouch.
Selecting pouches
Pouches can be transparent or opaque. Transparent pouches allow you to see the stoma postoperatively and allow patients to watch as they place the pouch over the stoma. Opaque pouches, of course, have the advantage of concealing the effluent.
Some pouches have filters. Colostomy patients usually prefer filtered pouches because they eliminate the need to burp the pouch to remove gas. Ileostomy output is usually watery, so the charcoal filters may get wet and quit working.
The appropriate type of pouch closure also varies, depending on the type of output and the patient’s needs and preferences. A patient with a colostomy or ileostomy needs a drainable pouch. Newer clamps and integrated closures can make closing the pouch easier for the patient.
Close-ended pouches are available for patients who empty their pouch once or twice a day. Reimbursement guidelines for Medicare, which most insurance companies follow, allow 60 close-ended pouches a month. Thus, someone who empties once or twice a day will have enough pouches.
Patients with urostomies use pouches with spigots on the end to allow for urine drainage.
Urostomy pouches can be connected to a continuous urinary drainage bag at bedtime or to a leg bag during the day for those in a wheelchair.
Dealing with complications
Report the following postoperative complications to the surgeon and the ostomy clinician caring for the patient:
• allergic reaction
• candidiasis
• contact dermatitis
• folliculitis
• ischemic or necrotic stoma
• mechanical irritation
• mucocutaneous separation
• parastomal hernia
• prolapse.
Many complications result from surgical technique or the patient’s disease status, but complications also result from an incorrect fit or an ostomy that frequently leaks. To determine why and where leakage occurred, examine the back of the barrier. If leakage results from a flush or recessed stoma or an irregular surface around the stoma, the patient may need a convex barrier. Or the patient may need a convex barrier and an ostomy belt.
Remember that a firm abdomen requires a soft, flexible barrier that conforms to the abdominal contours. A soft belly, on the other hand, may need the rigidity of a convex barrier to help the stoma empty into the pouch.
For weepy, extremely denuded skin, apply ostomy powder, brush off the excess, and dab an alcohol-free skin sealant, such as No-Sting by 3M, on the area. Allow the area to air-dry before applying the barrier.
Discharge planning and patient teaching
Because the postoperative length of stay is short, start preparing for discharge and teaching the pouch-change procedure at your first hospital encounter with the patient. Teaching the patient at each encounter creates a continuum of care throughout hospitalization and recovery. If possible, include the caregiver. (See Teaching your patient to change an ostomy pouch by clicking the PDF icon above.) Before discharge, give the patient two or three ostomy pouches to take home, step-by-step printed instructions on applying pouches, a list of supplies the patient will need, and a list of ostomy product suppliers in the area.
Also, teach the patient about complications, activity, diet, and drug therapy and provide the names of local support groups. (See Finding support by clicking the PDF icon above.)
Complications at home
Tell the patient to call the physician if any of the following occurs: fever, increased pain or discomfort, diarrhea, dehydration, or signs and symptoms of infection at the surgical site. The patient should also call the physician if there’s no output from the stoma for more than 24 hours.
Patients with urostomies who develop the following signs and symptoms may have a urinary tract infection: fever, chills, abdominal or retroperitoneal pain, and bloody, cloudy, or foul-smelling urine. Clear urine with mucus shreds is normal.
Increasing activity
Explain that after surgery the patient should feel a little bit stronger every day. Teach the patient to alternate rest and activity periods and to increase the activity period a little each day while building endurance. Refer the patient to the physician for clearance to resume exercise and sexual relations.
Dietary considerations
After ostomy surgery, your patient will start on a clear liquid diet and progress to a normal, preoperative diet. The patient should reintroduce one food at a time to help determine if it’s well tolerated. High-fiber foods should be introduced slowly.
Tell your patient to expect his or her body to tolerate the food as it did before surgery: if onions caused gas before surgery, they will do so after surgery, too, but the stoma will expel the gas. Make the patient aware of other gas-forming foods, such as hard-boiled eggs, spicy foods, fish, dried beans, carbonated beverages, and beer.
Tell the patient to chew food well and to drink plenty of liquids, which will prevent blockage. Explain the importance of hydration to avoid constipation, dehydration, and urinary tract infection. To prevent dehydration, ileostomy patients who are not on fluid restriction should drink 64 ounces of fluid a day. Teach these patients to replace fluids by drinking a glass of water every time they empty their pouches.
Drug therapy
Tell the patient to adhere to the prescribed regimen and to call the physician before using any new drugs. Instruct patients with ileostomies not to take laxatives because they may become dehydrated. These patients should tell their pharmacist that they have an ileostomy, so the proper form of prescription drugs can be ordered. Extended-release tablets will not break down in time and may be found in the pouch.
Rewarding work
Keeping up with the changes in ostomy equipment and care and teaching new ostomy patients the skills they need can be challenging. But helping these patients regain the confidence and learn the skills they need to improve their quality of life makes the rewards much greater than the challenges.
Selected references
Colwell J. Principles in stoma management. In: Colwell JC, Goldberg MT, Carmel JE, eds. Fecal and Urinary Diversions Management Principles. St. Louis, MO: Mosby; 2004:240-262.
Discharge Planning for a Patient with a New Ostomy: Best Practice for Clinicians. Glenview, IL: Wound, Ostomy and Continence Nurses Society; 2004.
Hampton BG, Bryant RA. Ostomies and Continent Diversions: Nursing Management. St. Louis, MO: Mosby; 1992.
McCann E. Common ostomy problems. In: Milne C, Corbett L, Dubuc D. Wound, Ostomy, and Continence Nursing Secrets: Questions and Answers Reveal the Secrets to Successful WOC Care. Philadelphia, PA: Hanley & Belfus, Inc; 2004.
The Sarah Cole Hirsh Institute for Best Nursing Practices Based on Evidence. State of the evidence review hospital to home: Planning the transitions. 2000; Cleveland, OH.
Goranka Paula Bak is an Ostomy Sales Territory Manager for Coloplast Corporation.
Read More