By: Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
The most basic principle of healing a wound is to determine the cause—and then remove it. This is easier said than done, as many wounds have similar characteristics and we don’t always know all the facts leading up to the wound.
The process has been unnecessarily complicated by the recent pressure (no pun intended) to avoid at all costs calling a pressure ulcer a pressure ulcer. I use the term “unnecessarily” because it doesn’t matter what it’s called—a pressure ulcer, decubitus, “de-cube,” or bedsore—because in the end, the general idea is it’s bad news.
So what’s behind the desire to avoid calling it a pressure ulcer? First, a pressure ulcer has traditionally been equated to poor nursing care. As Florence Nightingale, the “Mother of Nursing,” wrote:
“If he has a bedsore, it’s generally not the fault of the disease, but of the nursing.”
No one likes to feel that he or she gave poor care, and as more hospital complications data are available to the public, reports of complications such as pressure ulcers affect people’s perceptions—right or wrong—about the care a hospital delivers.
The second reason gets at the “at all costs” part of the desire. The recent attention given to Medicare’s “present on admission” rule and “never” events has
elevated pressure ulcers high up the chain of “no-no’s” and put the hospital at risk for nonreimbursement. And many private insurers have followed Medicare’s lead in denying coverage for pressure ulcers that occur in the hospital. Unfortunately, all the focus on reimbursement is beginning to challenge even the best wound care experts, who simply want to get the patient’s wound healed.
Pressure from upper management has resulted in experts trying to bargain and rationalize their way out of calling it what it is (a pressure ulcer), instead calling it a bruise, not a deep-tissue injury. Or saying, “This is a shearing ulcer, not a pressure ulcer.” Or, my favorite: “It’s not an ischial pressure ulcer but a diabetic ulcer because the patient is a diabetic.” Wound care experts are being forced to question and doubt themselves because money, quality assurance, and reputation are on the line when an in-house wound is labeled a pressure ulcer.
Like crime scene investigation, determining wound etiology requires us to gather all the facts. Once the facts are in, systematically comparing and contrasting the clinical findings aids differential identification to pin down the type of wound present. It’s important that we assess and investigate all the following when searching for the cause:
• patient’s medical history
• recent activities (such as surgery, extensive X-rays, or long emergency-
department waits)
• comorbidities
• specific wound characteristics, such as location, distribution, shape, wound bed, and surrounding skin.
Naming the wound is an important first step in intervening. If the wound is caused by pressure, call it a pressure ulcer and jump into action. Remove the cause, heal the wound, and prevent further breakdown. Don’t let yourself be influenced by those who aren’t experts in wound care.
Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Editor-in-Chief
Wound Care Advisor
Cofounder, Wound Care Education Institute
Plainfield, Illinois
Selected reference
Nightingale F. Notes on Nursing: What It Is, And What It Is Not. London: Harrison and Sons; 1859. http://ia600204.us.archive.org/17/items/notes
nursingnigh00nigh/notesnursingnigh00nigh.pdf.
Accessed August 30, 2012.


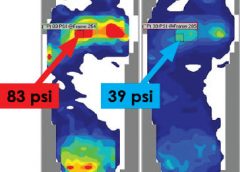



 Washington, D.C. – The National Pressure Ulcer Advisory Panel (NPUAP) announced the convening of its subcommittee, the Support Surface Standards Initiative (S3I), this spring to approve new standards tests that may help prevent pressure injuries in bed-bound individuals.
Washington, D.C. – The National Pressure Ulcer Advisory Panel (NPUAP) announced the convening of its subcommittee, the Support Surface Standards Initiative (S3I), this spring to approve new standards tests that may help prevent pressure injuries in bed-bound individuals. 


