By Kulbir Dhillon, MSN, FNP, APNP, WCC
Venous disease, which encompasses all conditions caused by or related to diseased or abnormal veins, affects about 15% of adults. When mild, it rarely poses a problem, but as it worsens, it can become crippling and chronic.
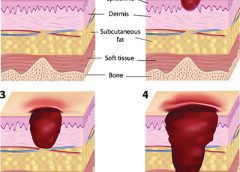
Chronic venous disease often is overlooked by primary and cardiovascular care providers, who underestimate its magnitude and impact. Chronic venous insufficiency (CVI) causes hypertension in the venous system of the legs, leading to various pathologies that involve pain, swelling, edema, skin changes, stasis dermatitis, and ulcers. An estimated 1% of the U.S. population suffers from venous stasis ulcers (VSUs). Causes of VSUs include inflammatory processes resulting in leukocyte activation, endothelial damage, platelet aggregation, and intracellular edema. Preventing VSUs is the most important aspect of CVI management. (more…)
Read More