By Ronald Rock, MSN, RN, ACNS-BC
Complex wound failures are costly and time-consuming. They increase length of stay and contribute to morbidity and mortality in surgical patients. Negative-pressure wound therapy (NPWT)—a common adjunct to wound-care therapy—is used to accelerate wound healing in all fields of surgery. Using a vacuum device and wound-packing material, it applies subatmospheric pressure to complex wounds.
But NPWT alone doesn’t ensure adequate wound healing. Many physiologic factors—including infection, excessive moisture, nutrition, and medications—influence wound-healing success. Failure to account for these factors or improper application of NPWT can limit patient outcomes and cause debilitating complications.
For clinicians, applying and establishing an airtight seal on a complex wound is among the most dreaded, time-consuming, and challenging NPWT-related tasks. Simply applying NPWT material under layers of transparent drape may delay wound healing or exacerbate the wound. This article provides tips on safe application of NPWT to enhance the outcomes of patients with complex wounds.
Consider wound location
Wounds on the body’s anterior surfaces are less susceptible to the forces of pressure, friction, and shear than those on posterior and lateral surfaces. Posterior and lateral wounds commonly require posterior offloading or repositioning the patient in bed to reduce or eliminate direct pressure. This can be done with judicious and frequent patient turning using a specialty bed or support surface.
Bridge a posterior or lateral wound to an anterior surface by placing the drainage collection tubing to a nonpressure-bearing surface away from the wound. Bridging keeps the tubing from exerting pressure on intact skin and decreases the risk of a pressure ulcer. To create the bridge, cut foam into a single spiral of 0.5 to 1 cm, or if using gauze, fold gauze into 8 single layers.
Place the spiraled foam or gauze layers onto the drape, ensure the bridge is wider than the collection tubing disc, and secure it with an additional drape. Next, apply the NPWT collection tubing on the end of the bridge away from the wound. A wide bridge under the collection tubing disc will minimize the potential for periwound breakdown when negative pressure is initiated. You may modify this spiraling technique by varying the width of the foam to fill undermining and wounds of irregular configuration and depth.
Protect the periwound
An intact periwound may break down from exposure to moisture, injury from repetitive removal of a transparent drape, or NPWT material coming in contact with skin. Skin protection is critical in preventing additional breakdown stemming from contact with potentially damaging material.
Transparent drapes are designed to permit transmission of moisture vapor and oxygen. Avoid using multiple layers of transparent drapes to secure dressings over intact skin, as this can decrease the transmission of moisture vapor and oxygen, which in turn may increase the risk of fungal infection, maceration, and loss of an intact seal.
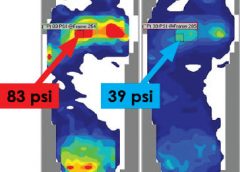
Periwound maceration also may indicate increased wound exudate, requiring an increase in negative pressure. Conversely, an ecchymotic periwound may indicate excessively high negative pressures. If either occurs, assess the need to adjust negative pressure and intervene accordingly. Reassess NPWT effectiveness with subsequent dressing changes.
Apply a protective liquid skin barrier to the periwound and adjacent healthy tissue to help protect the skin surface from body fluids. The skin barrier also helps prevent stripping of fragile skin by minimizing shear forces from repetitive or forceful removal of transparent drapes. Excessive moisture can be absorbed by using a light dusting of ostomy powder sealed with a skin barrier. A “window pane” of transparent drape or hydrocolloid dressing around the wound also can protect surface tissue from contactwith NPWT material and prevent maceration.
Avoid creating rolled wound edges
In the best-case scenario, epithelial tissue at the wound edge is attached to the wound bed and migrates across healthy granulation tissue, causing the wound to contract and finally close. With deep wound environments that lack moisture or healthy granulation tissue, the wound edges may roll downward and epibole may develop. Epibole is premature closure of the wound edges, which prevents epithelialization and wound closure when it comes in contact with a deeper wound bed. (See Picturing epibole by clicking the PDF icon above.)
Materials used in NPWT are primarily air-filled. Applying negative pressure causes air removal, leading to wound contraction by pulling on the wound edges—an action called macrostrain. Without sufficient NPWT material in the wound, macrostrain can cause the wound to contract downward and the wound edges to roll.
Ensure that enough NPWT material has been applied into the wound to enhance wound-edge approximation and avoid creating a potential defect as the wound heals. Before NPWT begins, material should be raised 1 to 2 cm above the intact skin. Additional material may be needed with subsequent changes if the NPWT material compresses below the periwound. The amount of NPWT material needed to remain above the periwound once NPWT starts varies with the amount of material compressed and the wound depth.
Reduce the infection risk
To some degree, all wounds are contaminated. Usually, the body’s immunologic response is able to clear bacterial organisms and wound healing isn’t delayed. But a patient who has an infection of a complex wound needs additional support.
Systemic antibiotics alone aren’t enough because they’re selective for specific organisms and don’t reach therapeutic levels in the wound bed. In contrast, topical antimicrobial adjuncts, such as controlled-release ionic silver, provide broad-spectrum antimicrobial coverage against fungi, viruses, yeasts, and gram-negative and gram-positive bacteria, including methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci.
Consider using controlled-release ionic silver for a wound known to be infected or at risk for infection due to its location or potential urine or fecal contamination. To be bactericidal, ionic silver must be in concentrations of at least 20 parts per million; also, it must be kept moist and must come in direct contact with infected wound bed. At lower concentrations, organisms may develop resistance. Ionic silver has no known resistance or contraindications. Dressings using it come in several forms, including a hydrogel sheet, perforated sheet, cavity version, and semiliquid hydrogel. Be sure the form you choose doesn’t occlude the NPWT material and compromise therapy. (See NPWT for a patient with necrotizing fasciitis by clicking the PDF icon above.)
View: NPWT
Obtain a negative-pressure environment
One of the most daunting aspects of NPWT is obtaining and maintaining a good seal—in other words, avoiding the dreaded leak. Preventive skin measures may contribute to a poor seal; skin-care products containing glycerin, surfactant, or dimethicone may prevent adequate adhesion of NPWT drapes. Body oil, sweat, and hair may need to be minimized or removed.
To avoid leaks, don’t overlook the obvious—loose connections, a loose drainage collection canister, exposed NPWT material, and skinfolds extending beyond the transparent drape. Tincture of benzoin (with or without a thin hydrocolloid dressing) increases tackiness to enhance the adhesive property of a transparent drape on the diaphoretic patient and on hard-to-drape areas, such as the perineum. But be sure to use tincture of benzoin with discretion, as it may remove fragile periwound tissue when the dressing is removed.
Ostomy paste products can serve as effective filler. These pliable products can be spread into position to obtain a secure seal under the transparent drape in hard-to-seal areas, such as the perineum. Pastes remain flexible and can be removed without residue. Temporarily increasing NPWT pressure to a higher setting may help locate a subtle leak or provide enough negative pressure to self-seal the leak. Once the leak resolves, remember to return the pressure to the ordered setting.
Knowledge optimizes healing
It’s important to be aware of potential complications of NPWT (See Take care with NPWT by clicking on the PDF icon above). However, when applied correctly, NPWT is an effective option for managing complex wounds. Recognizing and managing potential complications at the wound site, ensuring periwound protection, minimizing epibole formation, and preventing wound infection can result in a better-prepared wound bed and promote optimal healing.
View: NPWT case study
Selected references
Baranoski S, Ayello EA. (2012). Wound Care Essentials: Practice Principles. 3rd ed. Springhouse, PA; Lippincott Williams & Wilkins.
Bovill E, Banwell PE, Teot L, et al. Topical negative pressure wound therapy: a review of its role and guidelines for its use in the management of acute wounds. Int Wound J. 2008;5:511-529.
Sussman C, Bates-Jensen B. Wound Care: A Collaborative Practice Manual for Health Professionals. 4th ed. Baltimore, MD; Lippincott Williams & Wilkins; 2011.
Ronald Rock is an Adult Health Clinical Nurse Specialist in the Digestive Disease Institute at the Cleveland Clinic in Cleveland, Ohio.
Read More