By Bill Sullivan, Indiana University
Flesh-eating bacteria sounds like the premise of a bad horror movie, but it’s a growing – and potentially fatal – threat to people.
In September 2023, the Centers for Disease Control and Prevention issued a health advisory alerting doctors and public health officials of an increase in flesh-eating bacteria cases that can cause serious wound infections.
I’m a professor at the Indiana University School of Medicine, where my laboratory studies microbiology and infectious disease. Here’s why the CDC is so concerned about this deadly infection – and ways to avoid contracting it.
What does ‘flesh-eating’ mean?
There are several types of bacteria that can infect open wounds and cause a rare condition called necrotizing fasciitis. These bacteria do not merely damage the surface of the skin – they release toxins that destroy the underlying tissue, including muscles, nerves and blood vessels. Once the bacteria reach the bloodstream, they gain ready access to additional tissues and organ systems. If left untreated, necrotizing fasciitis can be fatal, sometimes within 48 hours.
The bacterial species group A Streptococcus, or group A strep, is the most common culprit behind necrotizing fasciitis. But the CDC’s latest warning points to an additional suspect, a type of bacteria called Vibrio vulnificus. There are only 150 to 200 cases of Vibrio vulnificus in the U.S. each year, but the mortality rate is high, with 1 in 5 people succumbing to the infection.
How do you catch flesh-eating bacteria?
Vibrio vulnificus primarily lives in warm seawater but can also be found in brackish water – areas where the ocean mixes with freshwater. Most infections in the U.S. occur in the warmer months, between May and October. People who swim, fish or wade in these bodies of water can contract the bacteria through an open wound or sore.
Vibrio vulnificus can also get into seafood harvested from these waters, especially shellfish like oysters. Eating such foods raw or undercooked can lead to food poisoning, and handling them while having an open wound can provide an entry point for the bacteria to cause necrotizing fasciitis. In the U.S., Vibrio vulnificus is a leading cause of seafood-associated fatality.
Why are flesh-eating bacteria infections rising?
Vibrio vulnificus is found in warm coastal waters around the world. In the U.S., this includes southern Gulf Coast states. But rising ocean temperatures due to global warming are creating new habitats for this type of bacteria, which can now be found along the East Coast as far north as New York and Connecticut. A recent study noted that Vibrio vulnificus wound infections increased eightfold between 1988 and 2018 in the eastern U.S.
Climate change is also fueling stronger hurricanes and storm surges, which have been associated with spikes in flesh-eating bacteria infection cases.
Aside from increasing water temperatures, the number of people who are most vulnerable to severe infection, including those with diabetes and those taking medications that suppress immunity, is on the rise.
What are symptoms of necrotizing fasciitis? How is it treated?
Early symptoms of an infected wound include fever, redness, intense pain or swelling at the site of injury. If you have these symptoms, seek medical attention without delay. Necrotizing fasciitis can progress quickly, producing ulcers, blisters, skin discoloration and pus.
Treating flesh-eating bacteria is a race against time. Clinicians administer antibiotics directly into the bloodstream to kill the bacteria. In many cases, damaged tissue needs to be surgically removed to stop the rapid spread of the infection. This sometimes results in amputation of affected limbs.
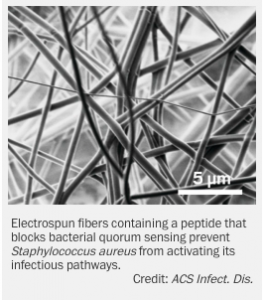
Researchers are concerned that an increasing number of cases are becoming impossible to treat because Vibrio vulnificus has evolved resistance to certain antibiotics.
How do I protect myself?
The CDC offers several recommendations to help prevent infection.
People who have a fresh cut, including a new piercing or tattoo, are advised to stay out of water that could be home to Vibrio vulnificus. Otherwise, the wound should be completely covered with a waterproof bandage.
People with an open wound should also avoid handling raw seafood or fish. Wounds that occur while fishing, preparing seafood or swimming should be washed immediately and thoroughly with soap and water.
Anyone can contract necrotizing fasciitis, but people with weakened immune systems are most susceptible to severe disease. This includes people taking immunosuppressive medications or those who have pre-existing conditions such as liver disease, cancer, HIV or diabetes.
It is important to bear in mind that necrotizing fasciitis presently remains very rare. But given its severity, it is beneficial to stay informed.
Bill Sullivan, Professor of Pharmacology & Toxicology, Indiana University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Read More