BY: NANCY MORGAN, RN, BSN, MBA, WOCN, WCC, CWCMS, DWC
What exactly is wound exudate? Also known as drainage, exudate is a liquid produced by the body in response to tissue damage. We want our patients’ wounds to be moist, but not overly moist. The type of drainage can tell us what’s going on in a wound.
Let’s look at the types of exudates commonly seen with wounds.
 Serous drainage is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing and smaller amounts is considered normal wound drainage. However, a moderate to heavy amount may indicate a high bioburden.
Serous drainage is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing and smaller amounts is considered normal wound drainage. However, a moderate to heavy amount may indicate a high bioburden.
Sanguinous exudate is fresh bleeding, seen in deep partial-thickness and full-thickness wounds. A small amount may be normal during the inflammatory stage, but we don’t want to see blood in the wound exudate, as this may indicate trauma to the wound bed.
Next we have the famous serosanguineous exudate, which is thin, watery, and pale red to pink in color. It seems to be everyone’s favorite type of drainage to document, but unfortunately, it’s not what we want to see in a wound. The pink tinge, which comes from red blood cells, indicates damage to the capillaries with dressing changes.
Seropurulent exudate is thin, watery, cloudy, and yellow to tan in color.
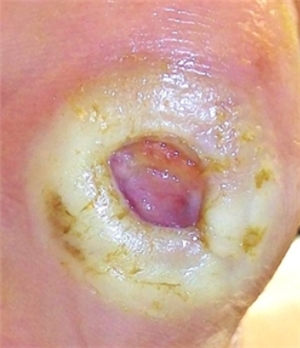
Purulent exudate is thick and opaque. It can be tan, yellow, green, or brown in color. It’s never normal in a wound bed.
So what types of drainage do you see being documented? The famous serosanguineous exudate? Are you really seeing drainage that indicates trauma to the wound bed, or is the drainage type mislabeled? Are you rethinking the need for a contact layer on the wound bed now?
DISCLAIMER: All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.







Hello,
I had a mastectomy 5 weeks ago. While most of the incision is healed, there is an opening which is producing large amouts of serous drainage requiring dressing changes twice a day. There is no infection and my surgeon says this is normal and will stop when the skin heals/closes. My concern is the length of time it has been and possibly will be, and the amount of exudate. The opening is a little larger than a quarter coin in size. Any comments or thoughts would be greatly appreciated!
Thank you,
Holly
Hi Holly,
I wish that I could give you a concrete answer on your wound here, but every surgical patient and surgical wound is different… my only advice is to keep the faith and continue to follow up with your surgical and wound care team! As with any wound that is slow to heal we always want to be sure that our patients are meeting their nutritional goals and if we as wound care clinicians aren’t getting the healing for our wounds that we would expect after a certain time frame, we might refer our patient for an advanced type of treatment/or modality to help speed things along if appropriate – hyperbaric oxygen therapy or negative pressure wound therapy for example. These are things you can always ask your surgical team or wound care team about and get more information on 🙂
Good luck!
I HAVE A PATIENT THAT HAS A VENOUS ULCER, ITS DRAINING GREEN EXUDATE, I AM USING ALGINATE SILVER TO THE WOUND AND USING COMPRESSING. WHAT DO U RECOMMEND
I had an gental infection in front and on the outer ,this is said to have been from my wife who has been strungling with verginal yeast for years now. It was inflamatory at first and now it has developed a wound on the urethinties this wound pass some yellow exudate which becomes think and closes the passing out of urine i am a male aged 45 . After cleaning it , it stats again what should i do for my healing
Hi Obrien,
It sounds like you still have some effects of the genital infection present. I would recommend you go to your MD immediately to get this re-evaluated as this could become worse and may need medical treatment/intervention. Good luck!
Nancy WCEI
I have a small wound on my feet due to the small bumps with water inside it, I pop it using a pin but after that I thought it was okay but it releases water everytime
Hi Judito,
I am not sure what kind of wound you have or what caused it but in general it is best not to “pop” blisters. The fluid inside the blister is filled with cells of repair and actually aide in the healing process. The experts say that it is best to leave it alone and let the body do its job. When we open or “pop” the blisters then we are creating away for bacteria to get inside and are putting ourselves at risk for infection. It really is best to leave the blister intact, let it “dry” up and reabsorb on its own without popping it. 🙂
Thanks,
Nancy WCEI
I had surgery to shave a tailor’s bunion and to remove the toenails off my big toes. Was in the ER om the 3rd, told I have cellulitis. On two antibiotics now. Noticed thin neon yellow line of exudate when changing nab dates on incision site? I don’t have another appointment until Thursday. Also, the big toe on the same foot is hurting more. Surgery was 12/17/13. Thanks
Hi
I have had 9 stitches on my ankle removed and still 1 week later it oozes sticky brown pus. I am on antibiotics.. But it doesn’t seem to be stopping. Although the cut was to the bone,is it normal to still be seeing this?
Sam not the norm at all glad you are seeing your MD on this and you are on antibiotics! Cause we don’t want this to infect the bone. I would follow up with your MD on this…..you should see it getting better not staying the same or getting worse.
I’m sorry to trouble you, but any help you can give me would be appreciated. I had a smash/crush injury (bite without broken skin) to my thigh in Feb. A hematoma apparently developed that was encapsulated and couldn’t drain but from the outside the area just looked badly bruised and swollen like a baseball. On 2/22, the 1st surgeon aspirated the hematoma but didn’t check for necrotic tissue, and when swelling returned in the area, 5 days later a different surgeon had to operate to remove the necrotic tissue (he cupped his hands like a baseball and said that was the amount of tissue he had to remove.) He placed a Jackson-Pratt drain in, which he removed two weeks later, but the wound site (about 8 inches long on thigh) keeps filling up. Since he took out the J-P drain, he has aspirated it with a needle once and removed 30 cc’s (on Wed.). Today is Friday and it has already completely filled up again. He is out of the office. My question is, is this normal and OK for it to fill up again so quickly? Do I just wait until Monday and don’t worry about it? Again, any help you can give me would be most appreciated!!
I have a total knee that was infected. had 7wks of IV antibiotics and now on oral. a]Now 4 months post op I have developed a serolus leak that unless elevated needs 2-4 dressing changes a day even though it is wrapped with ace bandage. Major worry is my lower leg at mid thigh are is 2 inches bigger than other. is this going to be permanent? and where does the fluid come from at this late post op stage?? and how is it going to be stopped. I can not sit all my life with leg elevated and do nothing.
I had a 1st compartment dorsal release 8 days ago. I have had multiple issues with nerve entrapment. The 2 inch incision has closed about 75% of incision line however in 1 are it has opened a hole even tho I still have internal stitches. It constantly has a white foam that bubbles out of it. There is no odor but it is a large amount. I cant seem to figure this one out. Help lol.
@Melody I would consult with your MD on this and keep your eye open for sign of infection which I see you are doing.
I have a new loop illeostomy and on top the margin has developed an abscess that is over 6 cm deep. It constantly drains and I can’t keep a illeostomy appliance on. I am suppose to be getting some aqua cel rope to pack with but now using me salt. I need help to keep the stool out and cover the abscess so the drainage will let a wafer stay.
@Julie aquacel rope is a good option to use it will absorb drainage and buy you longer wear time. They even have that with “silver” called Aquacel AG this would be used if you have any signs of infection locally in case stool got in there. Silver will help with bacteria load.
I have a small toe which has a discharge which looks like white chalk mixed in water. What is this? Could you help
@Elena do you have gout by chance?
i have once heard of this evisceration that can result in wound layers protruding through the skin,so can there be other means of controlling this effect and when does it really occur?
Evisceration is when separation occurs of all the incision/wound layers and may lead to the internal organs, usually the bowel, protruding through the open surgical wound – a very serious complication that requires immediate medical intervention. Prevention includes infection prevention and following post-op surgeon orders with lifting and splinting/bracing to support the incision line.
Plz help..my father 52 yeats old .4 weeks ago in a accident he have a wound on the leg neat the foot ..a clear fluid always runnig from the wound ..wound is deep and on accident docter stitched the wound but after seven days my family docter open the stitches wound open again ..now liquid runnig or a layer fill with water somtime occur on the wounds ..no sugar and blood test ok ..surgeon says its heal time by time ..what we do
@narinder-sounds like the surgeon wants to keep it open so it can drain, using dressings that can absorb drainage and keep your eyes open for any signs of infection. Keep following up with the surgeon. Hope all goes well.
Help… Have pt with pot ind 2012 removale of abess. Sacral Wound stage 2 positive for Morganella M. Have difficulties getting refferal to wound care at local hospital. I can get wound bed closed for a week then boom turn pt and attacked by seropurlent sanguinous exudate. Wound opening is very smalll almost pinpoint. Inflamation 1 to 2 inches around wound opening undermining and tunneling present. Currently using wet 2 dry with small amt of bactroban oint any advice would be much welcomed. I do suspect he needs another ind of wound there is alot of harden dark tissue also. It is at the point where i can predict when it will open again
Margaret what you posted tells me you need a consult on this cause your tx is not working and not lowering the bioburden. Consult Prescribing authority on using a antiseptic irrigation and packing and you are correct you might need some surgical help as well on this.
hello
my arm has been swollen for over 6 years from doing dialysis and having a fistula. i now have a transplant so no longer do dialysis but it remains swollen. fistula was dismantled. i have a blockage in my subclavian vein with 5 stents which causes the chronic swelling. recently i have noticed a scratch (probably from cat) on this arm and it has been oozing a slow clear fluid, very slight tinge yellow but mostly clear for almost 24 hours. its slow, but it wont stop. i am wondering what the cause of this might be and if i should be concerned? it has happened before on my arm but never for so long. it only ever happens on my swollen arm. does it have something to do with the swelling? thank u
I am now in a rehab. and have a roommate. I have Ph + CML leukemia, pulmonary fibrosis, asthma, gerd, high blood pressure, epilepsy, IBS-diarrhea, allergies to smoke and some medicine and sulfur, I have a pace maker, diabetes type 2, and a few other things I always forget. The roommate has enough drainage from her hip replacement that thought she wet her bed! She is eight days post surgery and two days and one night here. I am terrified of the amount of fluid coming out of her body! They change it two to three times a day and her bed is soaked as if she peed it. You see the things I have (and oh,I’m on oxygen told you I’d forget something) and with her obvious issues, do you know what I’m in for? Could she have Mersa or so other crap that will kill me? Do I at least need to be moved away from this person? Please help me!
My wound excretes a red semi liquid. I haven’t got a tt injection nor have I visited a doc. But the wound has dried up and there is pain only when I walk. I have been applying heated rock salt with coconut oil covered in a cloth on my wound. Is the discharge normal? What should I do if not?
I have a question…I had a distal pancreatectomy and splenectomy 6-7 weeks ago.post op day #7,my incision began draining tan purulent exudate…the MD determined it to be a “staph” infection and I had multiple doses of iv zosyn and then levaquin.I was hospitalized for 3 wks.I went home on Monday 2/8/16 with a wound vac and Home Health. The RN came on Wed and Fri that week….on Friday I noticed that the drainage was turning green becoming more viscous and developing an odor. She agreed and called my MDs nurse who
said that was “normal”. Over the WE it worsened…increasing in output as well as odor. The HH RN returned on Mon, and again agreed it was getting worse. Again she called my surgeons RN…..who,again said “that’s perfectly normal and fore to just keep my scheduled appt on.Fri. By Mpn night I felt increasingly ill having chills and nausea. At 11pm my husband took me to the ER. I was extremely hypotensive i.e. 80/68, 70/48. My heart rate was 120-150s, having chills and extreme abdominal distention….I was becoming septic. I was readmitted and 6 days later was found to be infected with Bacteriodes Fragilis….an anaerobic organism found in the gut so obviouslyy colon was.nicked allowing the bacteria to entery peritoneal cavity. I was on the hospital for 2 more weeks…went back to OR for “removal of infected tissue”& was advised I had a “pocket of infection and a pancreatic fistula. I was treated with oral Flagyl and am continuing it at home. A JP drain was placed to drain the fistula which has tan/watery drainage. My open incision has greatly diminished in size & the green exudate has greatly decreased as well……BUT THE POINT IS IM CONTINUING TO HAVE THE GREEN EXUDATE EVEN THOUGH I’VE BEEN ON Flagyl for 2 wks.My question is how am I going to determine when the infection is completely healed? Should I expect the drainage to completely stop? I’m afraid the incision will close
and trap the drainage inside.I’ve lost a great deal of confidence in my surgeon and his staff.
My 91 year old father had a basel cel carcinoma cut out of his head a couple of years ago, which did not heal. He then had some radiotherapy done last year which left a portion of his scull exposed. He is having the wound dressed by the nurses in his retirement home and I noticed there is still some pus after completing an anti-biotic. My question is how best to treat the wound.
1. He is in some pain following the cleaning and dressing of the wound. They applied a silver dressing with a thick wad of lint, plus waterproof outer. Is pressure required? Is it necessary to change it twice a week?
2. Should I ask for a stronger anti-biotic?
Hello-I had a wisdom tooth pulled a week ago. I can taste and smell this horrible liquid coming from the area where my tooth was taken out . My oral surgeon said its normal, but it’s starting to freak me out. I don’t know what’s worse, the smell of it, or the taste. When I look inside my mouth, there is what looks like a tooth still in the area where my wisdom tooth was pulled. My surgeon said that’s tissue and the whole will heal/close up Does any of this sound normal?
I had surgery three months ago and have had it splinted for three months the splint was taken off yesterday and the next morning it started leaking a reddish serum should i be alarmed.
2nd° burn -silvadene applied- do I cover it with a dressing?
i was cooking then I got a burn and it did had blisters then it popped. the problem is it got an infection and i am taking meds now. but i got a confusion on my wound. it is excreting green fluids and it got dry. i don’t know whether i will remove it the green fluid that is dry or just keep it there.
Hello everyone,
My mother is a 58 yo woman who just underwent a liver transplant 6/22/16. At her transplant clinic this past Monday (7/25/16), we brought it to the Dr attention that she had hard swelling under the incision on the right side. He sent her down for US, and they did a guided aspiration. I just looked at the report and it said:
“Under ultrasound, a pocket of complicated multi septated fluid was identified in the right paraumbilical area extending to the right flank beneath the healing surgical incision.”
“A 5 French, 10 cm catheter was introduced into the abdominal wall fluid collection under direct ultrasound visualization. 50 mL of serosanguineous fluid was aspirated.”
“1. Technically successful ultrasound guided abdominal wall fluid aspiration with collection of 50 mL of serosanguineous fluid.”
“2. Large complicated subcutaneous fluid collection. Difficult to aspirate completely secondary to the multi septated architecture.”
What does this mean? Is that on par with having a hematoma &/or serotoma, or is this something else?
Thank you.
Hello. I injured both of my nail beds on each big toe during an athletic event. The pain was intense initially and is starting to subside now at day 4. However, the nail beds are opaque with a bluish cast. They also began to seep a clear fluid, perhaps serous? My question is, should I use the heated pin/clip technique to create a small hole on the nail bed to relieve the pressure of fluid or is it best to let the body heal on it’s own? Does one offset the likelihood of losing the nail?