Skin substitutes (also called tissuebased products and dermal replacements) are a boon to chronic wound management when traditional therapies have failed. When selecting skin substitutes for their formularies, wound care professionals have many product options—and many decisions to make.
Repair of skin defects has been a pressing concern for centuries. As early as the 15th century BC, Egyptian physicians chronicled procedures and herbal treatments to heal wounds, including xenografts (skin from another species). The practice of applying allografts (human cadaver skin) to wounds was first documented in 1503. In 1871, autologous skin grafting (skin harvested from the the person with the wound) was tried. Next came epithelial- cell seeding, which involves scraping off the superficial epithelium of healthy skin and transplanting the cells onto the wound.
Today, skin grafting and seeding techniques are used successfully for treating wounds. Autologous grafts are the optimal choice for wound coverage. But availability of skin for harvesting may be limited, particularly in cases of large burns. Also, autograft procedures are invasive and painful.
Allografts and xenografts (for instance, porcine or bovine grafts) may be used as temporary skin replacements. Typically, though, these are later covered by an autograft. Also, they have significant clinical limitations, including immune rejection with allogeneic grafts (grafts from donors who are genetically different from the recipient but of the same species), as well as pain, scarring, slow healing, and infection.
Bioengineered skin substitutes
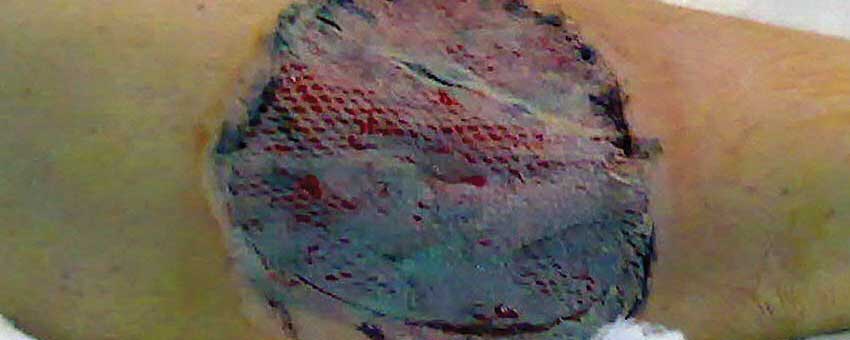
Bioengineered skin substitutes were created to eliminate certain problems with skin grafts. They’re used to treat non-healing wounds and for soft-tissue grafts in patients with life-threatening full-thickness (third-degree) or deep partial–thickness (second-degree) burns, surgical wounds, diabetic foot ulcers, venous ulcers, and certain other conditions, including epidermolysis bullosa. (See Skin substitutes for chronic wounds.)
Bioengineered skin substitutes contain live human cells that are seeded onto a matrix and provided with the proteins and growth factors needed to grow and multiply into the desired tissue. Various biosynthetic and tissue-engineered human skin equivalents are manufactured under an array of trade names and marketed for various purposes. Because these products are procured, produced, manufactured, or processed in different ways, they can’t be evaluated as equivalent.
Bioengineered skin substitutes fall into five classifications:
• cultured epithelial autografts
• human skin allografts derived from donated human cadaver tissue
• allogenic matrices derived from human neonatal fibroblasts
• composite matrices derived from human keratinocytes, fibroblasts, and bovine or porcine collagen
• acellular matrices derived from porcine or bovine collagen.
Some skin substitutes also possess unique regenerative properties. For instance, an allograft made of amniotic membrane and umbilical cord (NEOX®, made by Amniox Medical) exhibits the same biology responsible for propagating fetal regenerative and scarless wound healing. When transplanted into the adult wound environment, these placental tissues modulate inflammation and promote healing.
In a 2016 study of 32 diabetic foot ulcers by Raphael, an average of 1.68 NEOX applications resulted in a healing rate of 87.5%. A 2016 study by Caputo et al found that an amniotic membrane/umbilical cord allograft proved effective in treating complex diabetic foot ulcers with osteomyelitis; patients had a 78.8% healing rate after an average of 1.2 applications. In contrast, a 2002 study by Margolis et al found that only 32% of diabetic foot ulcers healed within 20 weeks of standard-of-care therapy (debridement, dressings, and topical ointment).
Choosing skin substitutes
Efficacy of skin substitutes varies widely in terms of the number of applications needed to close a wound, healing rates, and healing times. Dehydrated amniotic skin substitutes are convenient to store and use, but are less potent than cryopreserved amniotic/umbilical cord skin substitutes, which better preserve the structure and key biological signaling of fetal tissues to quickly promote revascularization in the adult wound bed. Choosing the skin substitute to match the desired clinical outcome is crucial. In addition, Medicare coverage varies considerably by region. (See How Medicare reimburses for skin substitutes.)
Ease of use and storage
Some skin substitutes require more maintenance than others, potentially leading to product waste if storage conditions aren’t optimal. For example, tissue-based products containing live cells have stringent shipping and application requirements; they’re shipped on dry ice and the patient must receive the graft within hours after the product arrives at the wound center. During an ice storm in Dallas, a truck delivering a tissuebased skin substitute for one of our patients had to wait out the storm on the side of the road; the patient cancelled his appointment due to impassable roads. By the time the patient rescheduled and the truck arrived with the skin substitute, the product was no longer usable and had to be thrown out.
In contrast, a skin substitute that remains stable in a wound center’s refrigeration unit is available when the patient needs it, so treatment can start sooner than with a product that has a narrow window for use. For instance, NEOX can be refrigerated safely at temperatures ranging from -112° to 39° F (-80° to 3.8° C) for up to 2 years without structural or functional compromise. If the product isn’t opened, it can be exposed to room temperatures of 68° to 77° F (20° to 25° C) for up to 6 hours and safely returned to cold storage. NEOX is the only cryopreserved amniotic membrane product that doesn’t need to be stored in a deep freezer.
Also, skin substitutes that require extensive preparation consume precious staff resources. One product, for example, needs to be washed in water at a temperature not exceeding 43° F (6.1 °C) before it can be applied to a patient’s wound. This requires an extraordinary effort for personnel in a busy wound clinic. Skin substitutes that can be exposed to room temperature before use are much more convenient and eliminate the need for special equipment, such as thawing tubs.
Disadvantages of skin substitutes
As an advanced tissue treatment modality, skin substitutes are more expensive than conventional wound dressings and may have more complex storage and preparation requirements. To prevent waste, clinicians should choose a product that can be stocked in a range of sizes. Some substitutes are available only in small or very large sizes, which don’t conform to most wounds; this means the wound center ends up paying for the excess product it must throw away.
Also consider how many times a skin substitute will need to be placed on a patient’s wound before it closes. One that needs to be applied only twice is more cost effective than a less expensive one that requires multiple applications. n
Myra Varnado is director of Clinical Wound and Ostomy Services for Corstrata, a national telemedicine company in Savannah, Georgia. Since 2000, she has been a member of the Wound Guidelines Task Force for the Wound, Ostomy and Continence Nurses Society (WOCN). Varnado is a primary author of WOCN’s guideline for management of wounds in patients with lower-extremity neuropathic disease. She is also a speaker and consultant for Amniox Medical, Inc., which markets the NEOX line of products.
Selected references
Amin N, Doupis J. Diabetic foot disease: from the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016;7(7):153-64.
Calota DR, Nitescu C, Florescu IP, et al. Surgical management of extensive burns treatment using allografts. J Med Life. 2012;5(4):486-90.
Caputo WJ, Vaquero C, Monterosa, A et al. A retrospective study of cryopreserved umbilical cord as an adjunctive therapy to promote the healing of chronic, complex foot ulcers with underlying osteomyelitis. Wound Repair Regen. 2016;24(5):885-93.
Cooke M, Tan EK, Mandrycky C, et al. Comparison of cryopreserved amniotic membrane and umbilical cord tissue with dehydrated amniotic membrane/ chorion tissue. J Wound Care. 2014;23(10):465-74, 476.
Doughty DB, McNichol LL, eds. Wound, Ostomy and Continence Nurses Society® Core Curriculum: Wound Management. Philadelphia, PA: Wound, Ostomy and Continence Nurses Society; 2015.
Halim AS, Khoo TL, Mohd, et al. Biologic and synthetic skin substitutes: an overview. Indian J Plast Surg. 2010;43(Suppl):S23-8.
Hill-Rom. 2016 International Pressure Ulcer Prevalence (IPUP) Survey. 2016.
Margolis DJ, Allen-Taylor L, Hoffstad O, et al. Diabetic neuropathic foot ulcers. Diabetes Care. 2002; 25(10):1835-9.
Nathoo R, Howe N, Cohen G. Skin substitutes: an overview of the key players in wound management. J Clin Aesthet Dermatol. 2014;7(10):44-8.
National Pressure Ulcer Advisory Panel. NPUAP Pressure Injury Stages. 2016.
Raphael A. A single-centre, retrospective study of cryopreserved umbilical cord/amniotic membrane tissue for the treatment of diabetic foot ulcers. J Wound Care. 2016;25(Suppl 7):S10-7.