LTC Stephen Rush joined the New York Air National Guard as a pararescue flight surgeon with the 103rd Rescue Squadron in 2007. His job was to train and sustain the medical readiness of PJs assigned to the 103rd. He became the medical director for all PJs in 2012.
“There are four main features to my role as medical director,” Rush says. “One is operational medical readiness, which includes writing protocols, how to teach them, how to keep the medical handbook current and disseminating the information to the units. Another role is human performance optimization. In some ways PJs are highly trained athletes, and I try to find the best ways to keep them physically healthy. So we do a lot of injury prevention and physical conditioning work. A third role is dealing with mental health issues, which are similar to issues with civilian first responders. And finally there’s dealing with the aerospace medical issues of PJs.
“Each PJ squadron has a flight surgeon assigned to fill these roles. Three years ago I created the pararescue medical director qualification course. Squadron flight surgeons have a wide variety of backgrounds and experience; some are general medical officers, a few are trauma surgeons, and some are board-certified emergency physicians. There was no central location to learn what a pararescue flight surgeon does. Each flight surgeon had to make it up as they went along.
“I traveled to different pararescue units to see how their flight surgeons performed, as well as U.S. Army Special Forces units and training schools to find out what their physicians were doing to train their medics. I then created a system to be used for consistent training for the PJs as well as training the flight surgeons. The medical director course covers those four main topics over a two-week period, including having them sit in on an NREMT paramedic refresher class that is operationally focused. We are about to institute an annual training program for the flight surgeons that will entail spending a week at a trauma center. In addition, we hope to set up some clinical requirements for PJs that would include time at a trauma center to allow them to do assessments and maintain their skills.
“Our PJs are spread out all over the world on training and operational missions. Some of those deployments can last for several months, so it’s challenging to keep track of what they’re doing. Now we’re in the process of developing a registry. The U.S. Army Rangers have a solid combat medical registry. I have a personal relationship with most of the PJ units, and they and their flight surgeons will let me know if they do something interesting that the other units might want or need to know. I’ve begun a podcast to discuss general issues and review cases and missions that have no operational security concerns. I started it to do 20 or so podcasts to cover our medical handbook; then I started to talk to different medical experts on different topics of interest and had them come on the podcasts with me. Now we’re also talking about general topics of interest, such as rescue missions from the past, leadership and mental health. The podcasts can be found on “PJ Medcast” on iTunes or pjmed.libsyn.com.
“We have a medical operations advisory board (MOAB) that meets annually to review policies and procedures. All our policies are created by expert consensus. In the pararescue medical community, we have a few surgeons and emergency medicine physicians. We also collaborate with the USAF trauma surgeons on policies, procedures, medications, etc. In addition, we get input from other military medical personnel and major civilian medical and trauma centers. For example, I have a very good relationship with the FDNY medical leadership. I’m happy to go to the experts, no matter where they are in the medical community. In addition, by going to the experts, I don’t have to do the research on something new or different—they’ve already done it.
“We also look at missions for lessons learned at the MOAB so all the units can benefit. And we don’t look at just the medical aspects. We look at mission planning, how the team was inserted, what equipment they used, etc. We look at the missions as a whole. We also discuss mental health and human performance optimization. The PJs have injury rates very similar to NFL and NHL athletes. The job is dangerous, and the training is dangerous. We are trying to reduce injuries and treat injuries in the best way possible. We use sports medicine principles and techniques to diagnose and treat injuries.
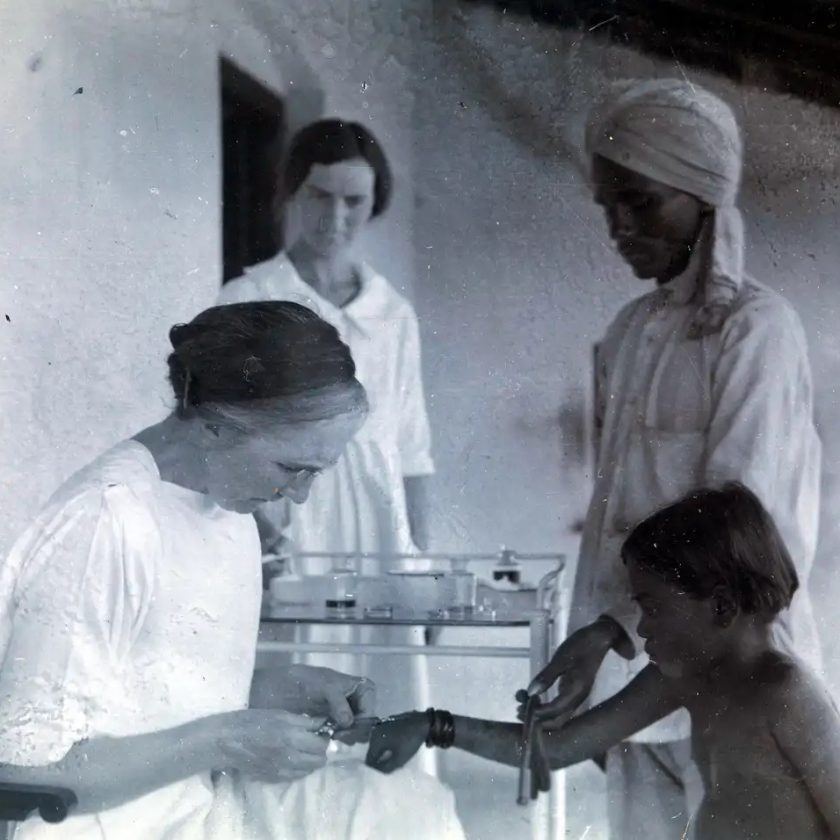
“Additional training for the PJs includes extended care when they may be with patients for several days. I look at rescue medicine as a distinct entity. The foundation of our medical training is the NREMT paramedic course. Then on top of that we add Tactical Combat Casualty Care, scuba-dive medicine, wilderness medicine, critical care transport, flight medicine, disaster response and humanitarian medicine. It’s a unique blend.
“As an example, when we parachute to a ship in the ocean, our most common patients have burns, acute abdomens and GI bleeds. Those things can lead to RSI, intubation, surgical airways, ventilator management and the use of blood products. We now jump routinely with red blood cells and plasma on these missions. We recently had a mission in the Atlantic Ocean with a burn patient with an inhalation injury and had to do a surgical airway; we had a good outcome. We teach the PJs the nursing care for extended missions such as hygiene and nutrition requirements for the patients as well as wound care. The PJs also have satellite communications with their flight surgeon, who may also include experts for treatment advice. We also make sure the PJs take care of themselves with proper nutrition, hydration and work/rest cycles.”