Negative pressure wound therapy (NPWT) uses negative pressure to draw wound edges together, remove edema and infectious material, and promote perfusion and granulation tissue development. The tissue stretch and compression created by negative pressure during NPWT promotes tissue perfusion and granulation tissue development through angiogenesis, cellular proliferation, fibroblast migration, increased production of wound healing proteins, and reduction of wound area. NPWT has been used to improve healing in a variety of wounds, including traumatic injuries, surgical wounds, pressure ulcers, diabetic foot ulcers, and venous stasis ulcers.
NPWT has now evolved to include automated instillation with dwell time (NPWTi-d, V.A.C. VERAFLO™ Therapy,KCI, an ACELITY Company, San Antonio, TX) that provides wounds with the benefits of both NPWT and wound irrigation. Wound irrigation is an effective, commonly used method to remove debris and infectious material as a means to promote wound healing. This article provides an overview of NPWTi-d.
Support for NPWTi-d
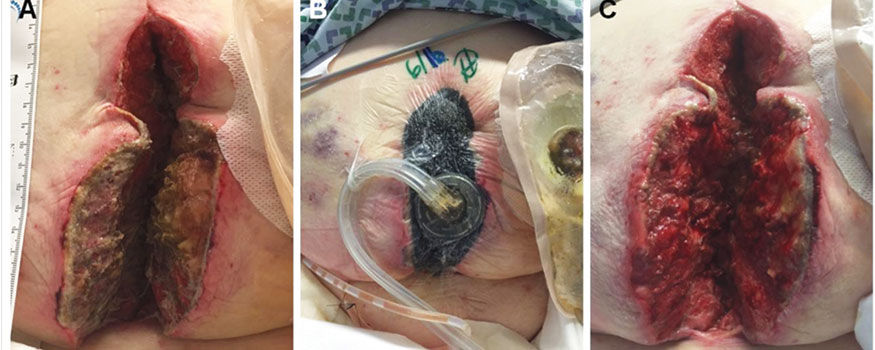
NPWTi-d has been used to treat many different wound types, including traumatic injuries, dehisced surgical wounds, pressure ulcers, diabetic foot ulcers, venous stasis ulcers, and burns. Studies report that NPWTi-d, compared to NPWT alone, decreases the number of surgical debridements, length of hospital stay, and length of treatment. These studies also report improved granulation tissue production and filling of undermined cavities. One study detailed the use of NPWTi-d as adjunctive treatment for bioburden management.
When to use (and not use)
NPWTi-d is primarily indicated for wound cleansing or to promote granulation tissue formation. (See Wound characteristics and NPWTi-d therapy goals.) NPWTi-d is contraindicated for patients with:
• a wound malignancy
• untreated osteomyelitis
• nonenteric and unexplored fistula
• necrotic tissue with eschar.
The treatment also shouldn’t be used with Octenisept® (Schülke and Mayr GmBH, Norderstedt, Germany), hydrogen peroxide, or alcohol-based solutions, or to deliver fluid into the thoracic or abdominal cavity because of the risk to alter core body temperature and cause fluid retention within the cavity. In addition, each wound should be thoroughly explored for intactness before starting NPWTi-d to avoid instilling topical solutions into adjacent body cavities.
Clinical considerations
Several wound irrigation solutions have been recommended for use with NPWTid. (See Instillation therapy settings). Common wound cleansers include normal saline, quarter strength (0.125%) or 0.0125% (one-tenth the concentration of quarter strength due to cytotoxicity) Dakin’s solution, super-oxidized water with neutral pH (Microcyn®, Oculus Innovative Sciences, Petaluma, CA), 0.5% sliver nitrate, and 0.01% polyhexanide (Prontosan® Wound Irrigation Solution, B. Braun Medical, Bethlehem, PA).
Concerns have been raised in Europe regarding polyhexamethylene biguanide (PHMB), a component of 0.01% polyhexanide. It was classified as a cancer-causing agent in concentrations of 1.0% or higher. However, 0.01% polyhexanide contains PHMB in extremely low concentrations (0.1%) diluted with betaine and purified water, so the carcinogenic classification does not apply.
Here are tips to ensure patients receive the optimal benefit from NPWTi-d:
• Become familiar with how to operate the pump. Getting used to the format may require a learning curve.
• Understand that NPWTi-d foam has higher tensile strength than traditional black NPWT foam to facilitate its easier removal from the wound bed and undermined cavities. It’s also less hydro – phobic, which helps to evenly distribute the wound irrigation solutions.
• For very large wounds, traditional black foam may be used in addition to the NPWTi-d foam to fill large wound cavities. If an additional drape is needed, a traditional drape may be used; however, the NPWTi-d drape is specifically designed to provide enhanced moisture-resistant adhesion along the wound edges to minimize irrigation solution leakage.
• In large wounds, it’s important to keep a running tally of the number of foams used. This will ensure their complete removal during dressing changes and when treatment has been completed.
• Periwound skin is fragile, so take care to protect it before treatment is started. Foam dressings should not come into contact with intact skin. Application of skin preparation products, an additional drape, hydrocolloid dressings, or transparent film over the periwound skin is recommended.
• Know that NPWTi-d can be used with bridging techniques if needed. Use careful attention to ensure the wound cavity is not overfilled, as additional irrigation solution will be required.
• Ensure a good seal because leaks could alter the amount of instillation volume and the negative pressure delivered to the wound and lead to a leak alarm. Apply gentle traction to skin creases and folds to obtain a flat surface for optimal drape adhesion. Apply the drape carefully, avoiding creases or puckering of the drape even in areas where they may overlap. Drape wrinkles may create small, unidentifiable passages for air to enter along the skin or in sections where the drape is overlapped into the foam as the negative pressure is initiated, which could cause a leak alarm. Applying a thin strip of additional drape along the existing edges or a silicone-based skin prep on the overlapped sections of drape may help achieve a good seal.
• Confirm that both the NPWTi-d cassette and canister are fully engaged and latched. Inappropriate placement or latching of the cassette and canister will cause errors in treatment application.
• Check that the NPWTi-d cassette tubing is not kinked, crimped, or blocked and that all clamps are open. This will allow the instillation fluid to be delivered easily into the wound bed.
• Remember that NPWTi-d canisters usually fill more quickly when combining wound drainage with the instilled solutions, so have extra canisters on hand to alleviate this problem. The unit will alarm when the canister is full.
• As the wound improves and the wound dimensions decrease, reduce the amount of solution instilled accordingly. Overfilling the wound may lead to a compromised seal and solution leakage.
• If possible, have an extra bag of prescribed irrigation solution on hand. Solutions other than normal saline will come from the pharmacy. Use quarter strength (0.125%) Dakin’s solution to minimize cytotoxicity. The pump will alarm when the solution bag is empty.
• Remember that you do not need to prime the line when spiking a new solution bag.
• Become familiar with the settings. The home screen on the unit will display the current NPWTi-d phase (Instill, Soak, or NPWT) with a timer indicating time remaining in that particular phase.
• Be aware of any discrepancy between the amount of prescribed solution instilled into the wound and the amount of solution returning into the drainage canister. Decreased or no return of solution may indicate transmission into an internal cavity. If this is the case, immediately stop instillation and notify the prescribing clinician.
• Understand that there is a learning curve with using NPWTi-d. Estimating the amount of solution to be instilled will vary. I have noticed a slight predisposition to overfilling. As such, I have taken 20% off the suggested instillation volume and continue to have success.
See Case study of NPWTi-d for an example of how this treatment can benefit patients.
An optimal patient experience
NPWTi-d helps remove infectious materials and promotes a wound-healing environment by combining the wound management benefits of NPWT and wound irrigation. Obtaining a complete drape seal, achieving appropriate attachment of canisters and cassettes, maintaining an open instillation solution line, and monitoring levels of fluid instilled and returned can contribute to a more comfortable patient treatment experience.
Ron Rock is the nurse manager and clinical nurse specialist for the WOC nursing team in the Digestive Disease Surgical Institute of the Cleveland Clinic in Cleveland, Ohio. R. Rock is a consultant for KCI, an ACELITY Company. The author thanks Julie M. Robertson, PhD (ACELITY) for assistance in the preparation and editing of this manuscript.
Selected references
Back DA, Scheuermann-Poley C, Willy C. Recommendations on negative pressure wound therapy with instillation and antimicrobial solutions – when, where and how to use: what does the evidence show? Int Wound J. 2013;10(1):32-42.
Gabriel A, Kahn KM. New advances in instillation therapy in wounds at risk for compromised healing. Surg Technol Int. 2014;24:75-81.
Gupta S, Gabriel A, Lantis J, et al. Clinical recommendations and practical guide for negative pressure wound therapy with instillation. Int Wound J. 2016;13(2):159-74.
Huang C, Leavitt T, Bayer LR, et al. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg. 2014;51(7):301-31.
Kim PJ, Attinger CE, Steinberg JS, et al. Negativepressure wound therapy with instillation: international consensus guidelines. Plast Reconstr Surg. 2013;132(6):1569-79.