http://www.sciencedaily.com/releases/2014/10/141016132852.htm
Read MoreCategory: Wound Care Advisor
Ramblings of an Itinerant Wound Care Guy
Renaissance and the New Golden Rule
by Dr. Michael Miller
To paraphrase Carol Ann from the Movie Poltergeist…”He’s Baaaaaaaaack” ! At the end of this past May, I had a sudden and disappointing parting of the ways from my prior blog host when I discovered the newest version of the Golden Rule…those that have the gold, make the rules. Is it possible to be too opinionated? Does the textual asbestos statement at the bottom of almost every web page regarding the dissociation between the hosts and the writer’s opinions really have any meaning? I am nonetheless extremely grateful to my prior hosts for allowing me the bytes to educate, illuminate and aggravate. The silent majority, mostly practitioners and patients who appreciate the inside story versus those with the gold (who don’t mind independent thinking, as long as it comes in their flavor of Kool-Aid) have both spoken.
But as PT Barnum said “’There’s no such thing as bad publicity’ and so, recognizing that more and more people are looking for a shoulder to cry on, a voice of reason, and the company that misery loves, “Ramblings of an Itinerant Wound Care Guy” re-emerges with this blog. I want to assure you that I have always relished comments and criticism both of which are proudly posted along with the blog, as long as you agree with me.
But enough fanfare and bravado and back to the bastion of wound dabblers anonymous. My three-month involuntary hiatus did little to quench the fires of indignation regarding medicine in general and wound care in particular. I had the great honor recently of meeting one of the creators of the wound care protocols for a large wound management organization. My initial disdain at our handshake turned to admiration as he explained with great pride, how the guidelines were created for diagnosis and care at their facilities. His background in wound care was impressive and his passion for care was the purest. However, in keeping with the mantra that “No Good Deed Goes Unpunished”, he related how his master plan had become intellectual oatmeal as the docs and nurses reverted to prior, Neanderthal practices. One of the major flies in his ointment was the fact that at least one facility under management had a huge number of men over 70 in treatment including hyperbarics with 100% having the diagnosis of venous insufficiency. Not a single mention of an arterial or diabetic etiology. When he brought it to the medical directors attention, the response was simply that was what had been diagnosed. He has since gone on to what he hopes are greener pastures. As far as the pitiful remnants of the wound caregivers he left behind, we agreed that they all deserve to be patient in their own centers.
To my prior readers who once again have elected to join in on the cacophony of intolerance or a newbie who on the advice of a friend decided to see what that crazy guy is writing about this month, I offer you my thanks and a promise to ignore the golden rule whenever and wherever I can. And by the way…the opinions of the statements made in this blog do not reflect those of the web site, the publisher or the editors…Got it.
Until we ramble next time.
Click here to return to Dr. Miller’s Ramblings of an Itinerant Wound Care Guy Blog page.
Disclaimer: The views expressed in this article are those of the author and do not necessarily represent the views of, and should not be attributed to, Wound Care Advisor. All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.
Read MoreWhite House declares war on drug-resistant superbugs
Clinical Notes: Wound Photography, Lymphedema, GI Complaints
Clinician Resources: Opioid-Prescribing, Diabetes, Pressure Injuries
Here are a variety of resources you might want to explore.
Considering opioid-prescribing practices
Healthcare providers’ prescribing patterns for opioids vary considerably by state, according to a report in Vital Signs from the Centers for Disease Control and Prevention (CDC). Here are some facts from the report:
• Each day, 46 people die from an overdose of prescription painkillers in the United States.*
• Healthcare providers wrote 259 million prescriptions for painkillers in 2012, enough for every American adult to have a bottle of pills.
• Ten of the highest prescribing states for painkillers are in the South. (more…)
Best of the best, the sequel
By Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
Welcome to our second annual “Best of the Best” issue of Wound Care Advisor, the official journal of the National Alliance of Wound Care and Ostomy (NAWCO). This may be the first time you have held Wound Care Advisor in your hands because normally we come to you via the Internet. Using a digital format for this peer-reviewed journal allows us to bring you practical information that you can access anytime, anywhere and gives you the ability to access videos and other links to valuable resources for you and your patients. (more…)
Read MoreInsulin use, dialysis predicted poor wound healing after endovascular therapy
Critical Wound-Healing Proteins Described
Burn Wounds Protected by Plastic-wrap-like nanosheets
Like cling wrap, new biomaterial can coat tricky burn wounds and block out infection.
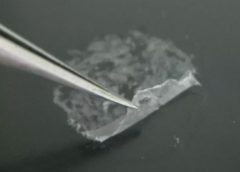
Wrapping wound dressings around fingers and toes can be tricky, but for burn victims, guarding them against infection is critical. Today, scientists are reporting the development of novel, ultrathin coatings called nanosheets that can cling to the body’s most difficult-to-protect contours and keep bacteria at bay.
The researchers are speaking about their materials, which they’ve tested on mice, at the 248th National Meeting & Exposition of the American Chemical Society (ACS), the world’s largest scientific society.
The meeting features nearly 12,000 presentations on a wide range of science topics and is being held here through Thursday. (more…)
Read MoreSage Products Introduces New Incontinence Clean-up Cloths
Saltier intravenous fluids reduce complications from surgery, study shows
Device–related pressure ulcers: Avoidable or not?
By: Donna Sardina, RN, MHA, WCC, CWCMS, DWC, OMS
A medical device–related pressure ulcer (MDRPU) is defined as a localized injury to the skin or underlying tissue resulting from sustained pressure caused by a medical device, such as a brace; splint; cast; respiratory mask or tubing; tracheostomy tube, collar, or strap; feeding tube; or a negative-pressure wound therapy device. The golden rule of pressure ulcer treatment is to identify the cause of pressure and remove it. Unfortunately, many of the medical devices are needed to sustain the patient’s life, so they can’t be removed. (more…)
Read More